Pressure sores: Prevention
What causes pressure sores?
Too much pressure on the same area can cause pressure sores (also called ulcers). Pressure causes a loss of blood flow and oxygen to the area, which can cause the skin and tissue cells to die. This occurs more often if your child is unable to move freely. Proper skin care and relieving pressure by shifting body weight can help prevent pressure sores.
What are the signs of pressure sores?
There may be one or more of the following:
- Skin redness that does not go away within 30 minutes after pressure is relieved.
- Change in skin color or temperature (warmer or cooler than other skin areas nearby).
- skin irritation such as a scraped area, break in the skin, blisters, or sores.
Where do pressure sores occur?
Pressure sores can occur in any area of the body, but boney areas are more likely to have problems. These include:
- head and ears
- shoulders and shoulder blades
- elbows
- hips
- lower back and tailbone
- knees and shins
- heels and ankles
Depending on your child's position, certain boney areas are more likely to have problems. (See pictures below.)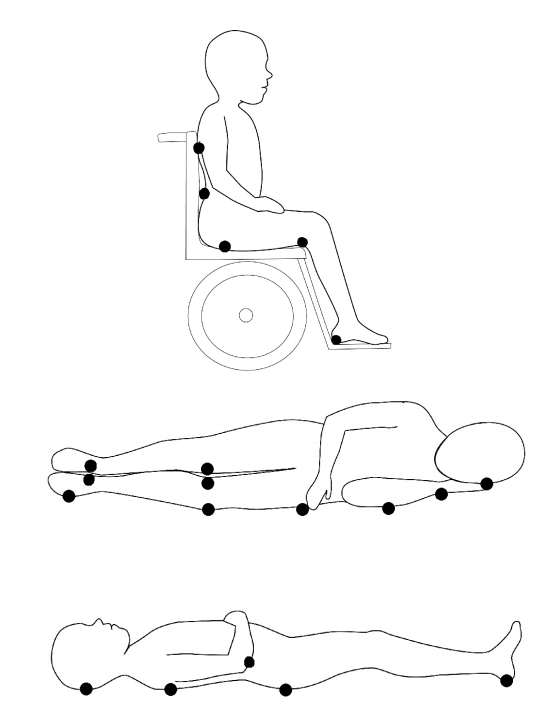
How can I prevent pressure sores for my child?
Your child's nurse, doctor, or rehabilitation therapist will teach you about specific care for your child. Some general guidelines are:
Hair and skin care
- Check your child's skin often for any of the signs of pressure sores – especially in the boney areas and skin folds.
- Protect boney areas from pressure. (See "Pressure reduction," on the next page.)
- Keep your child's skin clean and dry.
- Use lotions to prevent dry skin.
- Avoid tight fitting clothes that may rub against your child's skin.
- Keep bed linens dry – use changeable pads as needed.
- Avoid wrinkles in linens and clothes under your child.
- Anytime you lie on something hard, there is a chance you can develop a pressure sore. If your child will be lying in one spot for a while, remove any scalp braids, beads, hair binders, barrettes or extensions to prevent pressure sores.
Pressure redistribution
- Children usually move every 15 minutes when awake. When in bed, encourage your child to turn to a different position at least every 2 hours while awake.
- Use a schedule to turn your child if unable to turn without help. Ask your doctor if you should have a turning schedule at night.
- When you move your child, avoid friction caused by sliding or pulling across sheets or other surfaces. Friction can damage the skin, much like sandpaper would. Lift your child instead.
- When your child is sitting in a chair, encourage weight shifting at least every 15 to 30 minutes.
- Use pressure re-distribution surfaces such as cushions, special mattresses, and padding to support boney areas.
- Avoid donut type devices, which may increase pressure in some areas.
- Toilet-seat time should be less than 15 minutes.
Other ways to prevent pressure sores
- Give your child a healthy diet and plenty of fluids. Good nutrition helps keeps skin healthy.
- Teens should avoid smoking and alcohol; these can decrease circulation to the skin and cause a greater risk of skin problems.
When should I call the doctor?
Call your child's doctor if:
- Skin redness or color change lasts more than 30 minutes after changing positions.
- You notice new signs of skin irritation such as rashes, sores, blisters, or bruises.
- You have questions or concerns about skin care and treatment.
What else do I need to know?
Your child is more likely to have skin problems if there is a loss of feeling in parts of the body. These areas have less circulation, and your child will not be able to feel irritation, burning, or pressure.
- Try not to have an IV placed in the area.
- Be careful with hot liquids.
- Try to avoid heating pads, electric blankets, or other types of heat to the area. Warm water bottles are safer; they cool down, preventing the area from getting too much heat for too long.
- Protect the area from extreme weather temperatures.
Questions?
This is not specific to your child, but provides general information. If you have any questions, please call your clinic.
Children's Hospitals and Clinics of Minnesota
Last reviewed by WOCN 8/2015
This page is not specific to your child, but provides general information on the topic above. If you have any questions, please call your clinic. For more reading material about this and other health topics, please call or visit Children's Minnesota Family Resource Center library, or visit www.childrensmn.org/educationmaterials.
© 2024 Children's Minnesota
