Breastfeeding an infant with cleft lip
How does breastfeeding help my baby?
Breast milk:
- is more nutritious and easier to digest than formula
- gives immune protection not found in formula
- lowers risk of infections
- helps minimize allergies
- helps the digestive system mature; protects against some bowel problems
- lowers risk of Sudden Infant Death Syndrome (SIDS)
- promotes eye and brain development
- is more economical than formula
When you breastfeed:
- you create a special bond with your baby
- your baby's mouth and tongue coordination improves, which will help speech skills
- you burn more calories than usual
- your uterus may shrink toward its pre-pregnancy size more quickly
For more details, see the education sheet "Breastfeeding."
Can my baby breastfeed?
Babies with a cleft lip, but no cleft palate, can usually breastfeed. With a cleft palate, poor suction can make it very difficult. You can pump your breast milk and feed your baby with a special bottle provided by a feeding specialist or speech therapist.
Are there special benefits for babies with cleft lip or palate?
Babies with cleft lip or cleft palate tend to have more ear infections—and breast milk helps protect against these infections. The mother's antibodies are passed on to the baby in the breast milk. For an infant facing surgery, this is a real benefit.
Choking and milk leaking from the nose may occur. Breast milk is less irritating to the mucous membranes than formula, because it is a natural body fluid.
For babies with cleft lip, breastfeeding helps strengthen the face and mouth muscles, leading to more normal facial formation. This promotes better speech skills as the baby grows.
Other advantages of the breast over a bottle: The breast is more flexible than a bottle nipple, and molds itself to the shape of the lip and mouth. A breast offers a baby more control over positioning and milk flow.
Many infants need the extra closeness and interaction of breastfeeding. Infants suck for comfort as well as for food, and these
babies may not be able to use a pacifier very well.
A breast pump can boost your milk supply while you get started. Feel free to ask your health care provider or lactation specialist.
What challenges could my baby have with breastfeeding?
- trouble maintaining a good seal
- gagging and choking
- milk leaking out of the nose
- may prefer the side without the cleft
- may tire more easily and not nurse long enough to get the hind milk, which has the most calories
- weak suck
- non-rhythmic suck
- swallowing too much air
How can I help my baby breastfeed?
If your baby tends to choke and leak milk from the nose, the modified football hold or the straddle position may help.
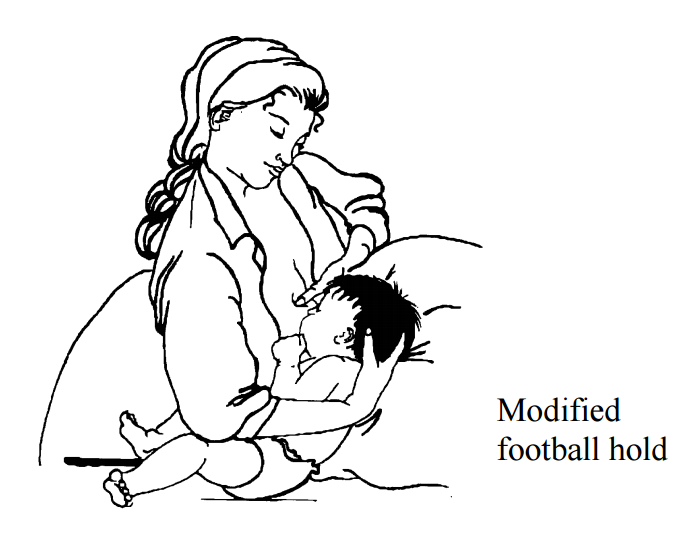
If your baby prefers one breast, try sliding the baby over to the other breast without turning. For example, feed in the cradle position on your left, then slide baby to the right and feed in the football position. If needed, use pillows for support.
Feed often, 8 to 12 times in 24 hours. You may need to wake your baby to feed. Look for mouth or hand movements. This usually means the infant is in a lighter sleep and can wake up more easily. Other ways to wake the baby: undress for a diaper change or make skin-to-skin contact.
Pump after feedings to empty the breast and stimulate milk production. If your baby does not start sucking, express some breast milk onto the nipple by hand or use a pump to get let-down started. This can encourage the infant to suck.
Once your baby starts sucking, look for jaw, ear, and temple movement. If not seen, the infant's suck is probably not as strong as it needs to be.
Sometimes the dancer-hand position (see picture below) can be used to support the infant's chin.
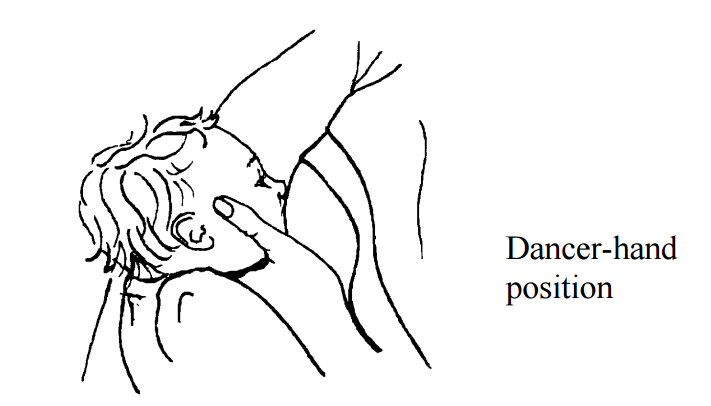
Slide the hand under your breast forward, so you are supporting the breast with 3 fingers rather than 4. Form a U-shape with your thumb and forefinger to cradle your baby's chin. This will help your baby press the nipple and areola between the gums.
If your baby has a non-rhythmic suck, try using a rocking chair. The baby who does not suck rhythmically may do better with extra chin support while breastfeeding.
Breastfeeding in calm surroundings with few distractions can help the infant who easily overreacts to stimulation.
How will I know my baby is getting enough milk?
Your baby should nurse every 2 or 3 hours (8 to 12 times in 24 hours), including some feedings during the night.
Watch for this pattern in your baby's stools during the first week after birth:
| Days after birth | Wet diapers (at least this many in 24 hrs) | Stool color | Number of stools (at least this many in 24 hrs) |
| 1st day | 1 | greenish-black | possible stool smears in first 24 hours |
| 2nd day | 2 | 1 to 2 stools | |
| 3rd day | 3 | stool turns yellower, softer, and seedier | 2 to 4 stools |
| 4th day | 4 | 3 to 5 stools | |
| 5th day | 5 | yellow, soft, seedy | 3 to 5 stools |
What else do I need to know?
Take care of yourself. You will be spending a lot of time each day feeding your baby. Patience is important.
Get comfortable before starting a feeding. Find a special place—perhaps where you can look out of a window. Cuddle and chat with your baby during each feeding.
Keep what you need at hand—maybe the phone and something to drink. You may want to listen to music or a relaxing program. If you are comfortable and well supported physically and emotionally, you will have more energy to support your baby.
Questions?
This sheet is not specific to you and your baby, but provides general information. If you have any questions, please talk to the nurse or lactation specialist.
At home, if you cannot tell if your baby is getting enough milk, or if you have other concerns, please call the clinic. If you need a pump or a lactation specialist, call:
Hollister at 1-800-323-4060, or
Medela at 1-800-835-5968.
La Leche League, International provides help and support to breastfeeding mothers over the phone and in support groups. For information, call 1-800-525-3243.
Children's Minnesota
Last reviewed 7/2021
This page is not specific to your child, but provides general information on the topic above. If you have any questions, please call your clinic. For more reading material about this and other health topics, please call or visit Children's Minnesota Family Resource Center library, or visit www.childrensmn.org/educationmaterials.
© 2024 Children's Minnesota
