Welcome to the Pediatric Emergency Medicine (PEM) fellowship program at Children’s Minnesota. You have chosen to explore one of the country’s premier PEM fellowship programs. Since 1989, we have trained fellows to be experts in the field of pediatric emergency medicine. We work hard to provide an environment where fellows gradually increase their confidence and medical knowledge, learn valuable management and teaching skills, and advance their understanding of clinical research.
Get details about the PEM fellowship
Get a look inside Children’s Minnesota
Learn more about what makes our program exceptional:
The Department of Pediatric Emergency Medicine is comprised of our staff physicians, nurse practitioners, and ancillary staff. We are one of the largest groups in the nation. Both of our main hospitals are staffed 24/7/365 with BC/BE PEM physicians. In addition to a complete array of pediatric subspecialists, we have numerous resources available in our emergency departments including interpreter services, social services, child life specialists, pharmacists, respiratory therapists and research assistants.
- Proudly sponsored by HealthPartners Institute in partnership with Region’s Hospital, home to one of the finest Emergency Medicine Residencies in the country. The Office of Health Professional Education at HealthPartners provides institutional resources and support to our program.
- Our PEM Fellowship provides the opportunity to work at both the Minneapolis and St. Paul Children’s campuses, which combined see more than 93,000 patient visits per year.
- Our Minneapolis campus is the only free standing children’s hospital in the region that provides level I trauma services in a pediatric-specific setting.
- Children’s St. Paul is the oldest children’s hospital in the state Regions Hospital serves as the training site for rotations in adult emergency medicine, emergency medical services and toxicology. It is a designated level 1 trauma center for adults and pediatric patients in St. Paul, and is known for its specialty care and Centers of Excellence led by highly skilled doctors, surgeons, rehabilitation specialists, nurses and staff members. Regions Hospital also serves as a Burn Center for St Paul and the east metro.
- Regions Hospital serves as the training site for rotations in adult emergency medicine, emergency medical services and toxicology. It is a designated level 1 trauma center for adults and pediatric patients in St. Paul, and is known for its specialty care and Centers of Excellence led by highly skilled doctors, surgeons, rehabilitation specialists, nurses and staff members.
- Our program includes 8-9 fellows, with support from over 40 board certified PEM physicians.
- Our Level I pediatric trauma center at Children’s Minneapolis is verified by the American College of Surgeons and is run in conjunction with our trauma surgeons and trauma physician assistants. Children’s Minnesota is the only freestanding level 1 pediatric trauma center in the state of Minnesota, as well as parts of western Wisconsin, North Dakota and South Dakota.
Our leadership
- Kara Seaton, MD – Fellowship Program Director
- Jennifer Argentieri, MD – Associate Program Director
- Kelly Bergman, DO – Associate Program Director, Research Director
- Heather Pomeroy, Fellowship Coordinator
Emergency department leadership
- Anupam Kharbanda, MD, MSc – Chief, Division of Critical Care
- Robert Sicoli, MD – Co-Medical Director, Department of Pediatric Emergency Medicine
- Valerie Whitcomb, MD – Ultrasound Director
Our fellowship program emphasizes the ACGME six core competencies (patient care, medical knowledge, practice-based learning, interpersonal skills, professionalism, and systems-based practice). The following goals will be accomplished through a variety of activities during the course of the fellowship:
Clinical
- Develop skills in initial assessment, resuscitation, stabilization and early management of pediatric emergencies.
- Gain broad knowledge and skills in common and uncommon pediatric emergencies.
- Become competent in the assessment and management of pediatric trauma.
- Master bedside ultrasound and understand its applications in pediatric emergency medicine.
- Acquire necessary skills in the field of adult emergency medicine and trauma.
Teaching
- Develop effective bedside and didactic teaching skills, for use with families, medical trainees, as well as teaching within the wider medical community.
- Learn to use Simulation as teaching tool for procedural competence and improving communication skills.
- Opportunities may include becoming PALS instructor and presenting and educating at conferences throughout the community.
Research
- Develop a foundation in the research process through formal training.
- Gain experience in grant writing, project development, paper presentation.
- Grasp basic concepts of statistics and epidemiology.
- Complete a written scholarly project, as required for board certification by the American Board of Pediatrics.
Administrative
- Understand the relationship of Emergency Medicine to hospital administration and committees.
- Become familiar with medical/legal issues, handling parent complaints, quality improvement, finances and scheduling.
- Understand state and regional administrative control of Emergency Medicine Systems.
Rotation curriculum
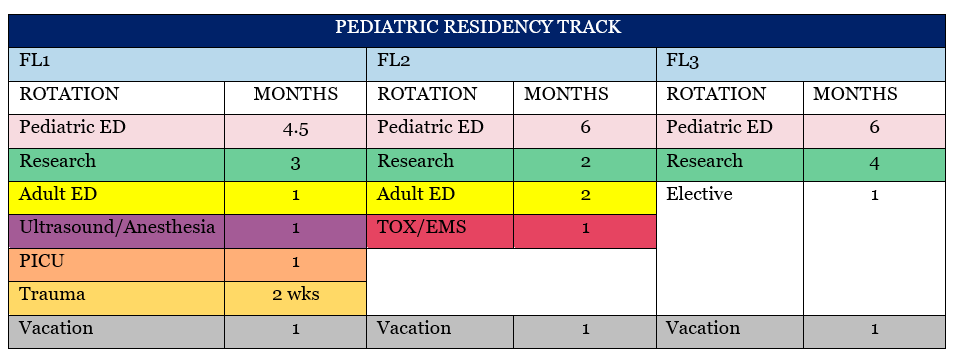
Fellows who have previously completed an EM residency operate on a two-year curriculum. Those who have completed a Pediatric residency function as a junior faculty in their second and third year. There is more than sufficient time and support to complete all requirements of the ABP and ACGME relevant to fellowship.
During emergency medicine rotations, fellows spend time in both of our pediatric emergency departments. Shifts vary to allow for diverse experiences, includes being an active participant and leader in traumas and medical resuscitations. In addition to standard shifts, fellows will have opportunities to complete ultrasound scanning shifts and procedure shifts to practice procedures such as suturing, foreign body removal, nail bed repairs and blocks.

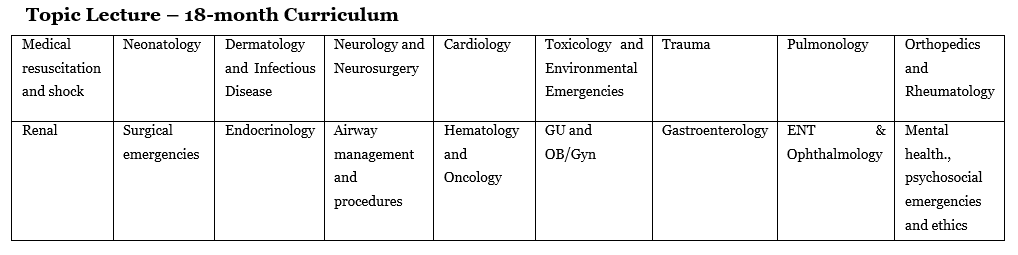
Didactics
Our fellows have protected education days every month. Some of our conferences are in collaboration with Region’s Hospital. Fellows have opportunities to teach or present cases at these conferences throughout the year.
Conferences
- Trauma Grand Rounds (combined with Region’s EM)
- Pediatric Critical Case Presentation (combined with Region’s EM)
- PEM Board Review
- Simulation
- Ultrasound teaching/skills
- Case Discussion
- PEM Journal Club
- Radiology Review
- Children’s PEM Staff Meeting Case Presentation
- Faculty/Fellow Lectures
- Research, Epidemiology and Statistics conferences
- University of Minnesota, Smiley’s Family Medicine Lecture (annually)
- Hospital-wide Disaster Drill Simulation (annually)
Additional training
Our fellows have the opportunity to attend a number of other training courses, conferences, national meetings, and credentialing courses. CME or Department funds are available to cover the cost of course fees, national meetings, certifications, and professional society memberships. We have adequate funds to cover travel to an additional conference (once annually). CME specific money is also available for textbooks and/or computer software (i.e. statistical programs, reference management software, etc.)
- Pediatric Emergency Medicine Fellow’s Conference
- Practical Emergency Airway Course (Dr. Levitan’s course)
- Children’s Minnesota Wound Management Course
- Academic meetings: PAS, AAP, ACEP, etc
- PALS, ACLS, ATLS, NRP
We seek physicians who have completed three years of training in a pediatrics or emergency medicine residency. Our PEM fellowship participates with the pediatric specialties fall match through National Resident Matching Program (NRMP).
We accept applications July 15–August 30 via ERAS. After completion of the application in its entirety, interviews will be offered to select applicants and scheduled accordingly. Interviews typically take place in September and October.
- Completed ERAs application
- Three (3) letters of recommendation, at least 1 from pediatric emergency medicine faculty
- Residency program director letter of recommendation and verification that applicant is in good standing
- One-page personal statement
- Results of USMLE testing
Please note: Our program is listed in FREIDA under our sponsoring institution, HealthPartners Institute / Children’s Minnesota. You may also search for us using our program ID (1142631025).
PEM fellows work closely with PhD biostatisticians, a Master’s level investigator (dedicated to helping ED fellows), clinical research coordinators (IRB and grant support), and research assistants (we employ a number of RAs for prospective data collection). We have numerous ongoing projects in our department and there are ample opportunities for our fellows to pursue their clinical interests. In addition, our site participates in the AAP Pediatric Emergency Medicine Collaborative Research Committee (PEMCRC), and the Pediatric Emergency Research Network (PERN). Motivated fellows have the opportunity to pursue projects within these research networks.
Academic faculty
A number of our faculty are dedicated to academics and have devoted time for clinical research and/or teaching. These faculty serve as mentors for fellowship projects, and will guide fellows through the process of project development, IRB submission, data collection and analysis, and final composition. Our main areas of research include point-of-care ultrasound utilization, management of diabetic emergencies, appendicitis, trauma, and measurements of social determinants of health. In total, our academic faculty have well over 100 publications. We are a highly motivated research group, and encourage fellows to submit their projects for publication.
Below is a list of our faculty in the Pediatric Emergency Fellowship program. Click on their names to view their profile.
Jennifer Ann Argentieri, MD
Joseph Leo Arms, MD
Kelly Bergmann, DO
Charles D. Blackwell, MD
Amy Borden, DO
Saydi Chahla, MD
Marydee C. Chamberlain, MD
Molly Curtis, MD
Anna Marie DePompolo, MD
Joanna Ekstrom, MD
Emilia Fisher, MD
Nita Gupta, MD
Jennifer R. Halverson, MD
Nihal Hamouda, MD
Thomas M. Hetzel, MD
David A. Hirschman, MD
Rosina Hussain-Weeres, MD
Vaishali Jha, MD
Adriana M. Klucar Stoudt, DO
Michelle Stacey London, MD
Manu Madhok, MD MPH
Laura Nilan, MD
Henry W. Ortega, MD
Jeffrey Jon Peterson, MD
David Piechota, MD
Robert Thomas Plouff, MD
Samuel R. Reid, MD
Tracy L. Ricke, MD
Meghann Ronning, MD
Annalisa K. Rudser, MD
Mark Gregory Schnellinger, MD
Kara Seaton, MD
Robert Alan Sicoli, MD
Thomas M. Skrypek, MD
Kellee A. Street, MD
Jennifer Thompson, MD
Marlike VanTyn, MD
Rachel Weigert, MD
Debra A. Weimerskirch, MD
Valerie T. Whitcomb, MD
Betty C. Wu, MD MPH
Class of 2024
Brian Lefchak, MD, MPH
Residency: New York-Presbyterian Weill Cornell Medical Center (Pediatrics)
Medical School: Drexel University College of Medicine
Taryn Raschein, MD
Residency: University of South Dakota Residency (Pediatrics)
Medical School: University of Minnesota Medical School
Bergthor Jonsson, MD
Residency: Mayo Clinic (Emergency Medicine)
Medical School: University of Iceland Faculty of Medicine
Class of 2025
Rachel Hedstrom, MD
Residency: University of Minnesota (Pediatrics)
Medical School: Eastern Virginia Medical School
Autumn Montville, MD
Residency: Mayo Clinic (Pediatrics)
Medical School: Chicago Medical School at Rosalind Franklin University of Medicine & Science
Class of 2026
Liz Chiquoine, DO
Residency: Rush University Medical Center (Pediatrics)
Medical School: Des Moines University College of Osteopathic Medicine
Tyler Ellis, MD
Residency: Mayo Clinic
Medical School: California Northstate University College of Medicine
Smrithi Krishnamohan, MD
Residency: Icahn School of Medicine at Mount Saini
Medical School: Pondicherrry Institute of Medical Sciences and Research
Faculty position after fellowship
Class of 2023
- Marshal Khant, DO (Mary Bridge Children’s Hospital – Tacoma, WA)
- Ariel Stein, MD (Children’s Minnesota – Minneapolis, MN)
- Devan Van Lanen-Wanek, MD (Maria Fareri Children’s Hospital – Valhalla, NY)
Class of 2022
- Joanna Ekstrom, MD (Children’s Minnesota – Minneapolis, MN)
- Tanya Paul, MD (Dayton Children’s Hospital – Dayton, OH)
- Alexandra Riggs, MD (Children’s Medical Center Plano – Plano, TX)
Class of 2021
- Emilia Fisher, MD (Children’s Minnesota – Minneapolis, MN)
- Rachel Weigert, MD (Children’s Minnesota – Minneapolis, MN)
Class of 2020
- Vivianne Tchonang Leuche, MD (University of Minnesota Masonic Children’s Hospital – Minneapolis, MN)
- Jonathan Nielsen, MD (University of Texas Southwestern – Dallas, TX)
- Normaliz Rodriguez, MD (John’s Hopkins All Children’s – St. Petersburg, FL)
Class of 2019
- Callie Becker, MD (University of Minnesota Masonic Children’s Hospital – Minneapolis, MN)
- Amy Borden, DO (Children’s Minnesota – Minneapolis, MN)
- Jennifer Thompson, MD (Children’s Minnesota – Minneapolis, MN)
Class of 2018
- Saydi Chahla, MD (Children’s Minnesota – Minneapolis, MN)
- Carly Theiler, MD (University of Iowa – Iowa City, IA)
- Gena Cooper, MD (University of Kentucky – Lexington, KY)
Class of 2017
- Meghan Cain, MD (Mayo Clinic – Rochester, MN)
- Michael McWay, MD (Children’s Hospital of Philadelphia – Philadelphia, PA
- David Piechota, MD (Essentia Health St. Mary’s – Duluth, MN)
Class of 2016
- Kelly Bergmann, DO (Children’s Minnesota – Minneapolis, MN)
- Meghann Ronning, MD (Children’s Minnesota – Minneapolis, MN)
- Jonathan Strutt, MD (University of Minnesota Masonic Children’s Hospital – Minneapolis, MN)
Class of 2015
- Anna DePompolo, MD (Children’s Minnesota – Minneapolis, MN)
- Kara Seaton, MD (Children’s Minnesota – Minneapolis, MN)
Class of 2014
- Leena Sastry, MD (Washington University of St Louis – St Louis, MO)
Contact us
Have questions about the Pediatric Emergency Medicine fellowship at Children's?