Abnormal Hemoglobins Beta Thalassemia Overview
People with Beta Thalassemia trait also can have a child with Beta Thalassemia disease. Beta Thalassemia disease is not a form of sickle cell disease, but it is a serious lifelong illness. People who have beta thalassemia disease do not make enough hemoglobin. The amount of hemoglobin a child can produce, determines whether a child has:
- Beta Thalassemia Intermedia
- Beta Thalassemia Major (also known as Cooley’s anemia).
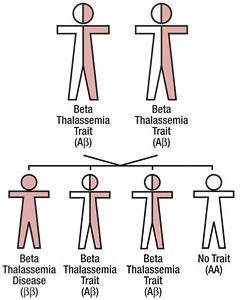
What if both parents have Beta Thalassemia trait?
If both parents have beta thalassemia trait there is a 25 percent (1 in 4) chance with each pregnancy of having a child with Beta Thalassemia disease. Beta Thalassemia disease is a lifelong illness that can result in serious health problems. These are the possible outcomes with each pregnancy.
- 25 percent (1 in 4) chance of having a child with beta thalassemia disease
- 50 percent (1 in 2) chance of having a child with beta thalassemia trait
- 25 percent (1 in 4) chance of having a child without trait or disease
Review – How Beta Thalassemia Trait, Beta Thalassemia Disease, and Sickle Cell Disease (Sβ Thalassemia Disease) are inherited
If one parent has beta thalassemia trait and the other parent has normal hemoglobin, there is a 50 percent (1 in 2) chance with each pregnancy of having a child with beta thalassemia trait.
If one parent has beta thalassemia trait and the other parent has sickle cell trait, there is a 25 percent (1 in 4) chance with each pregnancy of having a child with sickle cell disease (Sickle beta thalassemia disease). Sickle cell is a lifelong disease with serious health problems.
If both parents have beta thalassemia trait, there is a 25 percent (1 in 4) chance with each pregnancy of having a child with Beta Thalassemia disease. Beta thalassemia disease is a lifelong illness with serious health problems.
The only way to know if you have beta thalassemia trait, is to have a simple blood test.
Talk to your physician about genetic testing and counseling if you or a member of your family member has beta thalassemia trait.
We know how difficult a diagnosis of thalassemia can be, both for your child and for your whole family. That's why our physicians are focused on family-centered care: From your first visit, you'll work with a team of professionals who are committed to supporting all of your family's physical and psychosocial needs. We'll work with you to create a care plan that's best for your child.
If your child has been diagnosed with thalassemia, you'll naturally be eager to know how your child's physician will treat it. Your child's physician will determine a specific course of treatment based on several factors, including:
- your child's age, overall health and medical history
- the specific type of thalassemia
- any complications your child has experienced
- your child's tolerance for specific medications, procedures or therapies
- how your child's doctors expects the disease to progress
Treatment
Treatment for thalassemia depends on the subtype of the disorder, but may include:
- Treatment for anemia based on severity
- Children with thalassemia may receive blood transfusions in order to treat the symptoms of anemia.
- Transfusions provide healthy blood cells from a donor. This can alleviate the symptoms caused by your child's unhealthy hemoglobin.
- Treatment for the effects of blood transfusions, such as iron overload.
Iron overload assessment
- Children who need frequent blood transfusions build up excess iron in their bodies, which can cause severe complications including liver and heart damage.
- To monitor iron levels in the body, children with severe thalassemia must undergo specialized imaging tests.
- At Children's, we offer advanced imaging techniques including FerriScan and T2* that help us monitor your child's iron levels and decide when chelation therapy is necessary.
- Thalassemia patients who require regular red blood cell transfusion gradually become iron overloaded.
- Without removal of this iron by chelation, it can become toxic to several vital organs.
- Children may take chelators orally or by injection in order to remove excess iron from the body.
Will my child require long-term care?
For children with more severe forms, thalassemia is a life-long condition requiring ongoing management. Your child will require regular follow-up in order to properly manage the disease and keep him healthy, including monthly blood transfusions.
Children with thalassemia intermedia should also receive follow-up to monitor symptoms of anemia.
We understand how overwhelming a diagnosis of thalassemia major (the most severe form of transfusion-dependent thalassemia) can be, especially because most children are diagnosed as infants. Right now, you probably have a lot of questions. How dangerous is this condition? What is the very best treatment? What do we do next?
We’ve tried to provide some answers to those questions in the following pages, and our experts can explain your child’s condition fully when you meet with us.
Beta Thalassemia - Internet Links For Families
These are available in several languages at the internet sites
An Introduction to Beta Thalassemia Trait:
http://cooleysanemia.org/updates/TI3.pdf
An Introduction to Beta Thalassemia:
http://cooleysanemia.org/updates/TM2.pdf
What is Beta Thalassemia Trait?:
http://cooleysanemia.org/updates/BetaEnglish.pdf
What is Beta Thalassemia Intermedia:
http://cooleysanemia.org/updates/TI3.pdf
Hemoglobins H:
This page is not specific to your child, but provides general information on the topic above. If you have any questions, please call your clinic. For more reading material about this and other health topics, please call or visit Children's Minnesota Family Resource Center library, or visit www.childrensmn.org/educationmaterials.
© 2024 Children's Minnesota