By: Robin Menier
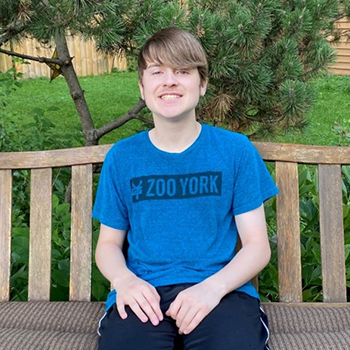
Our son Ben was admitted on Wednesday, April 1, 2020, due to a hole opening up along his incision line on his head. Two years ago, he was in a car accident and suffered numerous injuries including a severe traumatic brain injury.
We had just started the distance learning for school and he mentioned to me that there was a really itchy spot on his skull that was bothering him a lot. I took a look and could see something black. I brought him over to the window and saw more closely that it looked like a piece of metal with a hole in it. I didn’t know what to do; I didn’t know what the situation was like at Children’s Minnesota at that time. All I had been seeing and hearing at that time was about New York and how the hospitals were full and they were having to create makeshift rooms, etc. I didn’t know if we should wait to hear back or if we should just get in the car and go to the emergency room.
I called the staff lead for the Families as Partners Program in full panic saying there was a hole in his head but I’m scared to go to the emergency department (ED) I asked: Were there a lot of people there? Would I be exposing him to more illness? Immediately she was able to calm me with the information about how quiet it was on campus and that everyone was wearing masks and that people were doing everything they could to make sure that patients and families felt comfortable bringing their kids in with emergencies like this.
A trip to Children’s Minnesota
Shortly after my freak out, the neurosurgery department at Children’s Minnesota called back after viewing the photos I sent. We totally lucked out that it was the same nurse practitioner (NP) and same neurosurgeon who treated him during his 7-week stay in 2018. They told us to come in the next morning and to pack a bag “just in case” he needed to be admitted.
We came in the next morning with our masks on and were so caught off guard by how quiet and empty the campus was. We were so used to all of the hustle and bustle. But the limited amount of people on campus also put us at ease since there was so little known about COVID-19 at that time. We saw the NP briefly, and she sent us over to the ED for bloodwork and his COVID-19 test. We were also completely surprised that there was nobody in the ED waiting. It felt so odd to be honest.
We were trying to keep things light for Ben, but it was a little scary to see the staff in all the levels of gear–gowns, masks and face shields. The nurse on call was fantastic: she explained the protocol of what she was wearing and why, she explained how things were different (i.e. lounges were closed) so she would get us water, the cafeteria was closed, so we were given a meal ticket for the parents too, and she explained the changes that could happen about the surgery prep too. I felt a little helpless.
Ben’s surgery
Instead of us accompanying Ben down to surgery, the anesthesiology team came to our room in their garb and explained that my husband and I should wait here in the room and that Ben would be brought back after the surgery. It felt a bit weird to basically stay in this room at all times, but we also understood this was all being done for the safety of the patients and the staff too.
In order to preserve PPE, Ben’s neurosurgeon called us from the nurse’s station phone and talked to us through the window. I so appreciated how much time he spent answering our questions and discussing any concerns we had. We also felt like we were doing our part in preserving PPE for patients that needed it more than we did. With all the concerns and questions that had to be going on during the early days of the pandemic, the staff was just as amazing as they were when we spent 7 weeks there in the PICU in 2018. It still felt like we were experiencing the best of the “Children’s way of doing things” and that we could feel confident in the care Ben was receiving.