Breastfeeding your hospitalized baby
Article Translations: (Spanish) (Hmong)
We support your breastfeeding goals. During your baby's hospital stay, nurses and lactation (breastfeeding) specialists can help you with any problems or concerns.
Your baby was born to breastfeed
Your baby was born with reflexes and instincts that help him to breastfeed. For example, when your baby's cheek or lips are stroked, he will open his mouth wide and search for your breast. This is called the rooting reflex. Two other reflexes that help with eating are the suck and swallow reflexes.
Another reflex that your baby may use to help him find the breast is the step reflex. After delivery, he could creep up your body and locate your breast, attach, and start to breastfeed.
Your breastfeeding experience may have been delayed or interrupted because of your baby's hospitalization. Breastfeeding is also a learning process for you and your baby. It may take some time for you and your baby to adjust. Even a mom and her healthy full-term baby usually need 2 to 4 weeks to become an efficient breastfeeding couple.
Here are some ideas that will help your baby and you succeed at breastfeeding.
- Build your milk supply with frequent emptying of your breasts. Mothers with generous milk supplies are more likely to have a baby that succeeds at breastfeeding. Empty your breasts at least 8 times per 24 hours, so that you will have a large milk supply.
- Hold your baby as much as possible. Research shows that frequent skin-to-skin contact or "Kangaroo Care" helps breastfeeding advance more quickly.
- Breastfeed when your baby is awake and alert. If baby is too sleepy, talk to your baby's doctor about when to supplement breastfeeding.
- If you are comfortable, your baby is more likely to be comfortable. Find a chair that fits you well and use pillows and a footstool to help the chair support your body.
- Please watch a 5-minute video on latch that you can find at http://www.ameda.com/breastfeeding/breastfeeding-videos
- Some breastfeeding videos available at Children's are A Premie Needs His Mother Volume 2, A Visual Guide to Breastfeeding and Follow Me Mum.
Breastfeeding holds:
Find a comfortable position for both you and baby while breastfeeding. We have some examples shown below, but you may need to find some variations specific to your breast and body.
Here are some tips:
- Let your breast lay in its natural resting position.
- Bring your baby to your breast.
- Your baby's ears, shoulders and hips should be in a straight line. There should be no twisting of the body or the neck.
- Your baby's face should be directly in front of the nipple and your nipple should touch your baby's upper lip.
- Your baby's body and hips should be pressed as close to you as possible.
- Your baby's head will tip back in a "sniffing position" before he attaches to your breast.
Cross cradle hold
This position is useful for preterm infants and other babies that have low muscle tone.
- Turn baby on one side to face you, with his tummy and hips touching your body.

- Support the lower part of your baby's head, the neck, and back with your palm and arm. Your inner elbow will keep your baby's hips tucked close to your side. Use pillows under arm as needed.
- Compress your breast behind the areola so baby can latch deeply onto the breast.
Football hold
This is another good position for preemies or other babies needing more neck support. Mothers with large breasts may also find this a useful position.
- Support baby's neck and back with your hand and arm. Tuck your baby's body and legs under your arm.

- Slide baby's bottom backward until it is pressed up against the back of your chair. Baby's legs should tilt up or be tucked at a right angle to his body.
- You may also hold your baby with his tummy facing your side and his legs will wrap around your ribs and back.
Cradle hold
This hold works best for a healthy full term baby or an older baby. A mother with very large breasts may have difficulty holding her breast in this position.
- Place baby's head on the middle of your forearm. You may need to position your baby's head closer to your wrist.

- Baby is on her side, chest to chest with mother. Keep baby's hips tucked close to your side.
- Older babies may breastfeed well with their head in the crook of the mother's arm.
Lying down (side-lying)

- Lie on your side with a pillow supporting your back and another pillow between your legs. Bend your knees as needed for comfort and support.
- Position baby on his side next to you to nurse. Bring your baby's hips close to your body. A rolled-up blanket placed behind the baby's back may help. Baby's nose will be at the level of the nipple.
Latch-on
Latch refers to the way a baby is attached to the breast. A shallow latch is when a baby only grasps mother's nipple. This causes baby to get small drinks of milk and may cause painful breastfeeding.
A deep comfortable latch is the goal. When baby has a wide-open mouth with her lips on mother's areola (dark area surrounding the nipple) she probably has a deep latch and can remove milk easily.
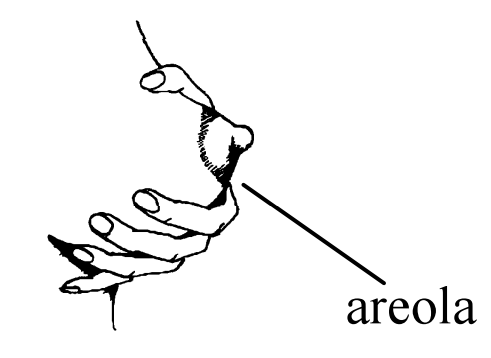
Gently stroke your baby's upper lip and mouth with your nipple until he or she opens wide!
If your baby's mouth does not open wide, rest your nipple on your baby's upper lip between strokes. Be patient! Babies know where to latch by smelling your scent and also by being in contact with your breasts.
When your baby opens as wide as a yawn, quickly pull your baby's shoulders closer to your body.
- Baby's mouth should be wide open with the tongue resting over bottom gum line.
- Part or all of your areola will be in the baby's mouth.
- More of your areola may be showing above your baby's mouth.
- Baby's lips, chin and cheeks touch your breast.


How do I know if my baby has a good latch?
Every time your baby sucks, you will feel a deep pulling sensation on your nipple. With the first few sucks, there may be some momentary discomfort. If you have long lasting pain that doesn't improve when your baby is re-latched, ask for lactation help. Pain may be warning sign.
You should hear a swallow after every 1-2 sucks. When your baby releases your breast, your nipple should be rounded and slightly longer.
If your nipple looks pinched, pointed, or angled like the tip of a new tube of lipstick your baby has a shallow latch and may have difficulty drawing milk from your breast. Your nipple may also hurt when this happens and will gradually become injured.
How often and for how long should baby breastfeed?
Babies can show feeding readiness behaviors that signal Mom to send food soon! These behaviors or feeding cues include:
- Hand-to-mouth
- Mouth and tongue movements
- Increased activity, waving arms & legs
- Crying is the last feeding cue
Babies should eat as soon as they are showing feeding cues. Babies usually breastfeed every 2 or 3 hours, or 8 to 12 times in 24 hours. Wake your baby if she or he sleeps longer than 4 hours, even at night, until advised by the doctor or lactation specialist.
At each feeding, let your baby suck as long as swallowing continues. Then move to other breast if baby still wants more. Some babies may nurse on both sides; others prefer only one side per feeding. The average length of a feeding is up to 30 minutes.
To remove your baby from your breast, place a finger in the corner of the mouth gently breaking the suction. Do not remove baby from your breast without breaking the suction first.
How do I arouse my sleepy baby for feeding?
Preterm, jaundiced and other babies recovering from an illness or surgery are often sleepy. They may not awaken often enough to eat and may lose weight or not gain adequate weight. As these babies mature and recover from their illness, they will be awake for longer periods.
Babies need to eat at least 8 or more feedings in 24 hours. If your baby is not awakening by himself to eat that often, you must help her. If a baby is deeply asleep and not moving, she may be very difficult to awaken.
- During baby's sleepy phase, watch for signs of eye or body movements. Your baby is easiest to arouse when showing some activity.
- Skin-to-skin contact can help arouse a sleepy baby.
- Talking to your baby, massaging and applying lotion are all ways to awaken your baby.
- You may want to try to express a few drops of milk onto baby's lips to coax the baby to your breast and to open her mouth.
How can I help my baby stay latched?
Some mothers have found that if they mold their breast into an oval shape or "breast sandwich," their baby is able to stay latched.
Your hand should be placed on the breast so that your thumb is parallel with your baby's upper lip and your fingers should be positioned parallel with the lower lip. Where you place your hand on your breast varies with your baby's position. The videos mentioned earlier show this.
How will I know my baby is getting enough milk?
- Baby breastfeeds every 2 or 3 hours (8 to 12 times in 24 hours), including some feedings during the night.
- You hear or feel your baby swallowing when your milk has released (after 1-2 minutes of breastfeeding).
- You feel a deep pulling sensation while baby is breastfeeding
- Your breasts feel softer after feeding.
- Your baby is gaining ½ -1 ounce per day or 4 to 7 ounces per week.
- Your baby is sleepy and satisfied after feeding
Watch for this pattern in your baby's urine and stools during the first week after birth:
| Days after birth | Wet diapers (at least this many in 24 hrs) | Stool color | Number of stools (at least this many in 24 hrs) |
| 1st day | 1 | Greenish-black, tarry, sticky | Possible stool smears in first 24 hours |
| 2nd day | 2 | 1 to 2 stools | |
| 3rd day | 3 | Stool turns green, then yellow, softer, seedier | 2 to 4 stools (green) |
| 4th day | 4 | 3 to 5 stools | |
| 5th day | 5 | Yellow, soft, seedy | 3 to 5 or more stools |
Questions?
This sheet is not specific to your child but provides general information. For more information, call the Lactation Consultants at:
Children's - Minneapolis 612-813-7654
Children's - St. Paul 651-220-7126
Children's Hospitals and Clinics of Minnesota
Last reviewed 8/2015
This page is not specific to your child, but provides general information on the topic above. If you have any questions, please call your clinic. For more reading material about this and other health topics, please call or visit Children's Minnesota Family Resource Center library, or visit www.childrensmn.org/educationmaterials.
© 2024 Children's Minnesota