Who will be on my care team?
At Midwest Fetal Care Center, a collaboration between Children’s Minnesota and Allina Health, we specialize in individual attention that starts with you having your own personal care coordinator to help you navigate your baby’s complex treatment process. We use a comprehensive team approach to spina bifida. That way, you are assured of getting the best possible information by some of the most experienced physicians in the country. For spina bifida treatment, your care team will include a maternal-fetal specialist, a pediatric surgeon, a neonatologist, a geneticist, a nurse specialist care coordinator, a fetal care clinical social worker and several other technical specialists. This entire team will follow you and your baby closely through the evaluation process, and will be responsible for designing and carrying out your complete care plan.
Meet the team
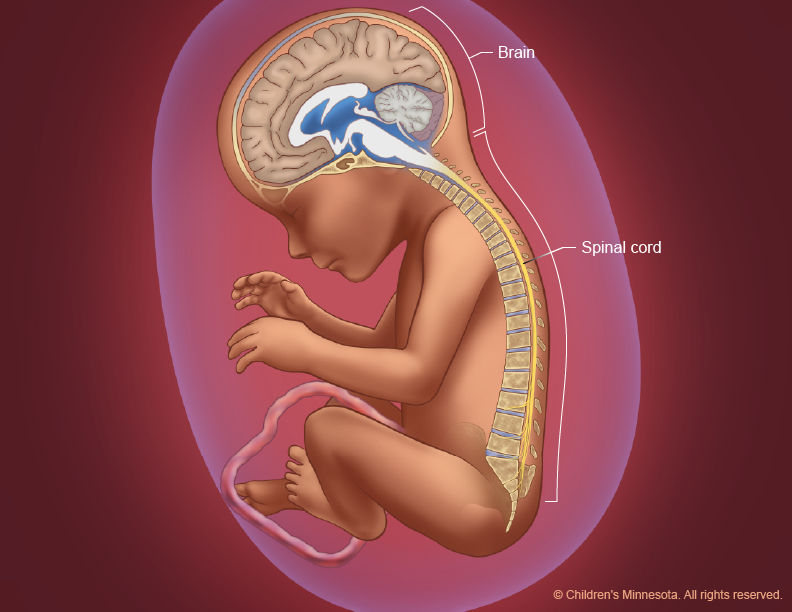
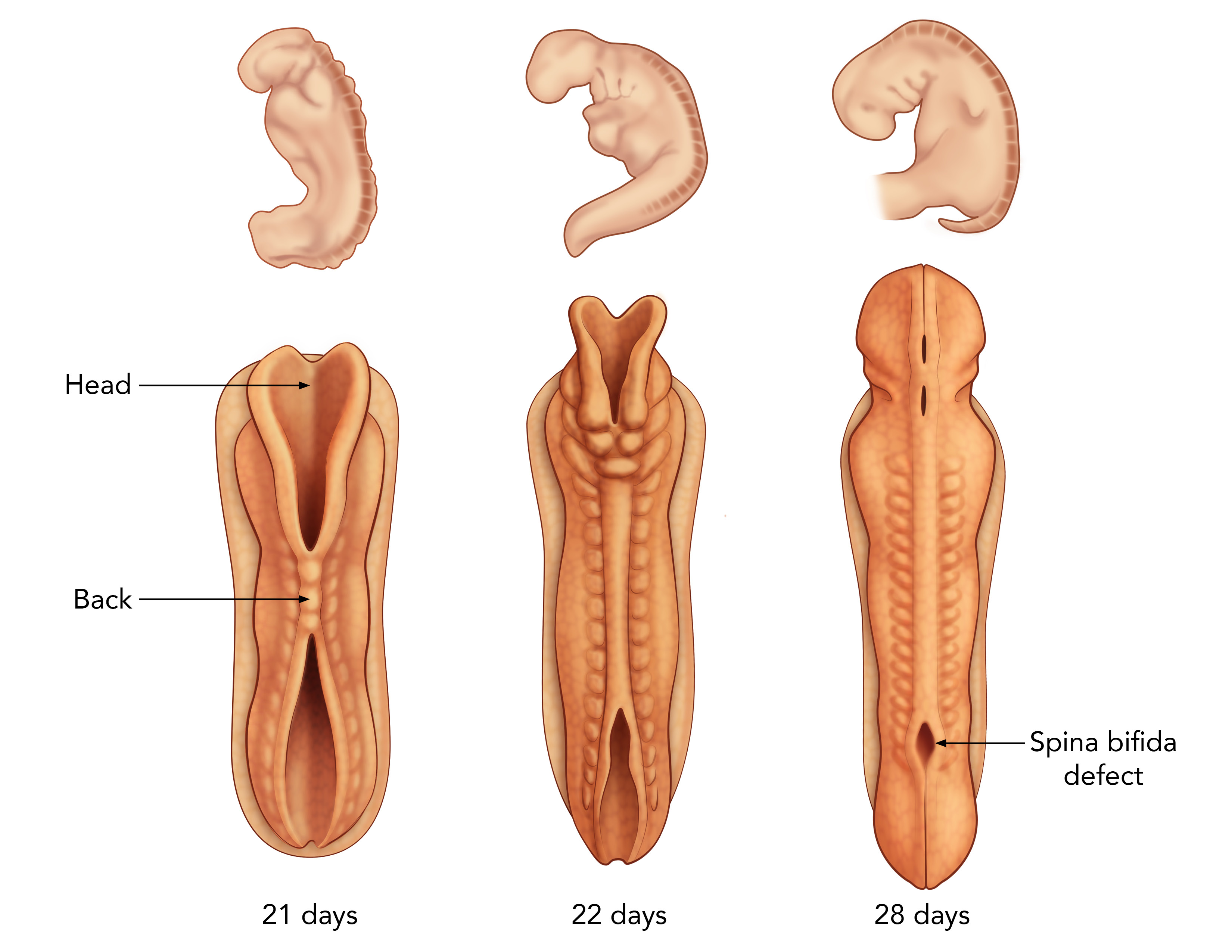
What causes spina bifida?
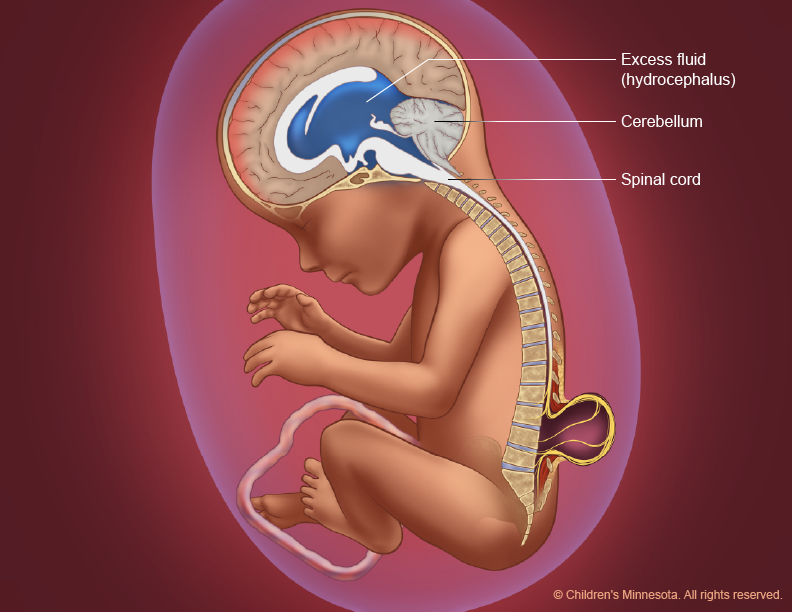
Spina bifida is the most common birth defect involving the central nervous system, occurring in about 1 in 3,000 live births. It’s believed to be caused by a combination of genetic and environmental factors. Women who have had one child with spina bifida have a 4 percent chance of having another child with the condition.
How is spina bifida diagnosed?
Spina bifida is readily detected by ultrasound. The condition is often first suspected, however, when a routine blood test — the maternal serum alpha fetoprotein (MSAFP) screening — produces abnormal results early in pregnancy. If spina bifida symptoms are suspected, your doctor will refer you to a fetal care center, such as the Midwest Fetal Care Center, for a diagnostic evaluation. At the Midwest Fetal Care Center, our evaluation process is comprehensive. It includes high-resolution fetal ultrasonography, fetal magnetic resonance imaging, amniocentesis testing and fetal echocardiography.
What is maternal serum alpha fetoprotein (MSAFP) screening?
This is a blood test that measures the level of alpha-fetoprotein (AFP) in the mother’s blood during pregnancy. AFP is a protein produced by the baby. A small amount of it normally crosses the placenta and enters the mother’s bloodstream. The most common reason for abnormal levels of AFP in the mother’s blood is a mistaken due date, but such abnormalities can also be a sign of a birth defect, including spina bifida. MSAFP screening is part of the routine screening that that women are offered starting the 15th week of their pregnancy.
What is high-resolution fetal ultrasonography?
If MSAFP screening indicates abnormal AFP levels, your doctor will suggest a high-resolution fetal ultrasonography exam. This is a non-invasive test performed by one of our ultrasound specialists. The test uses reflected sound waves to create images of the baby within the womb, including the baby’s spine. The images can help detect signs of abnormal openings in the spine.
What is fetal magnetic resonance imaging (MRI)?
Fetal MRI is another non-invasive test. It uses a large magnet, pulses of radio waves and a computer to create detailed images of your baby’s spine and other structures while in the womb. This procedure involves both mom and baby being scanned while partially inside our MRI machine. The test is a bit loud, but it takes about 30 minutes and is not uncomfortable.
What is amniocentesis?
If your baby is found to have spina bifida, your doctor will offer you an amniocentesis test to see if your baby has any associated genetic or chromosomal condition that would exclude him or her from being a candidate for spina bifida surgery in utero. This test is a necessary part of the evaluation process when prenatal surgery is being considered. For this procedure, a small sample of fluid will be removed from the amniotic sac surrounding your baby. The amniotic fluid will contain cells from your baby, and in those cells will be your baby’s chromosomes for us to analyze. The procedure is straightforward and can be done in our clinic. It requires placing a small needle through the abdomen and into the amniotic sac to obtain the fluid sample. Test results will take several days for our laboratory to process.
What is fetal echocardiography?
Fetal echocardiography (“echo” for short) is performed at our center by a pediatric cardiologist (a physician who specializes in fetal heart abnormalities). This non- invasive, high-resolution ultrasound procedure looks specifically at how the baby’s heart is structured and functioning while in the womb. This exam is important because babies with spina bifida may be at increased risk of heart abnormalities. A fetal echocardiogram is also a necessary part of the evaluation process when prenatal surgery is being considered.
How is spina bifida treated?
Spina bifida treatment depends on many factors, including the severity of the condition. At Midwest Fetal Care Center and Children’s Minnesota, we offer all spina bifida treatment options available for the care of babies with spina bifida, including prenatal and postnatal surgery. Our multidisciplinary care team will help you understand the diagnosis of spina bifida so that you can make the best treatment decision for your child.
Prenatal surgery for spina bifida
What is prenatal surgery for spina bifida?
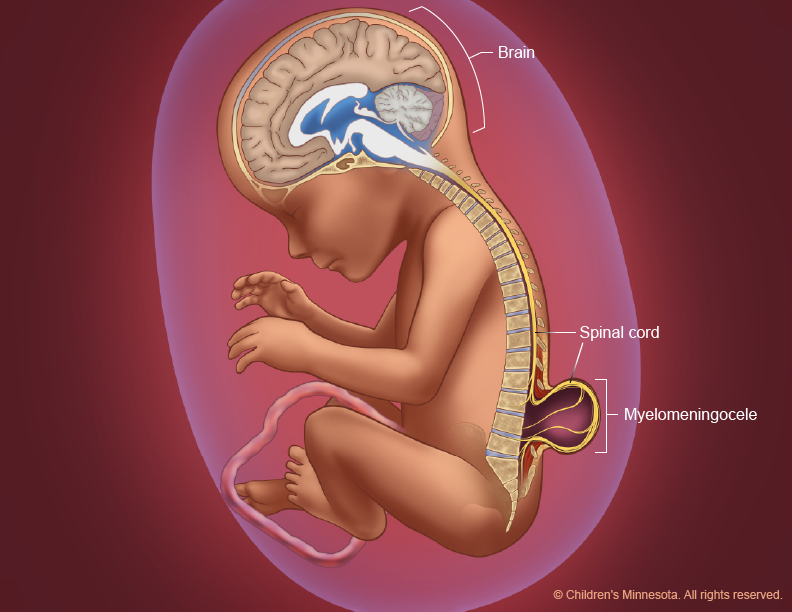
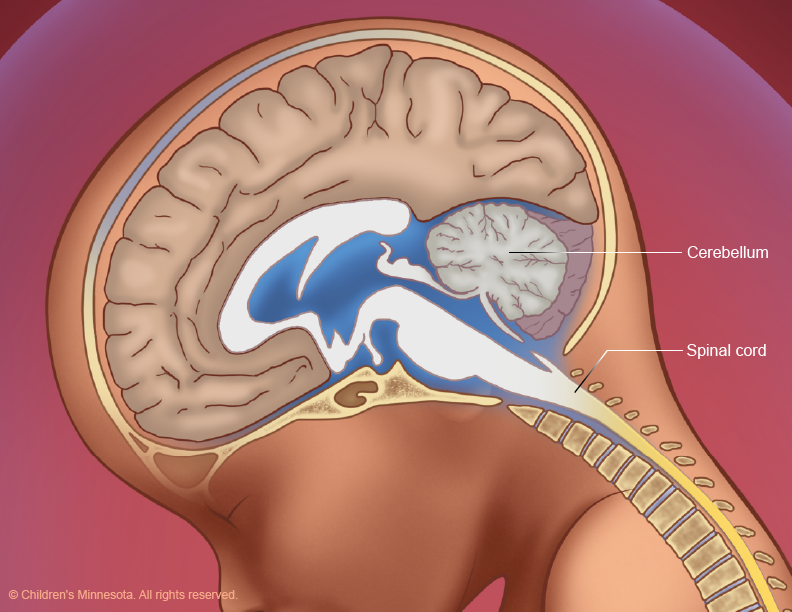
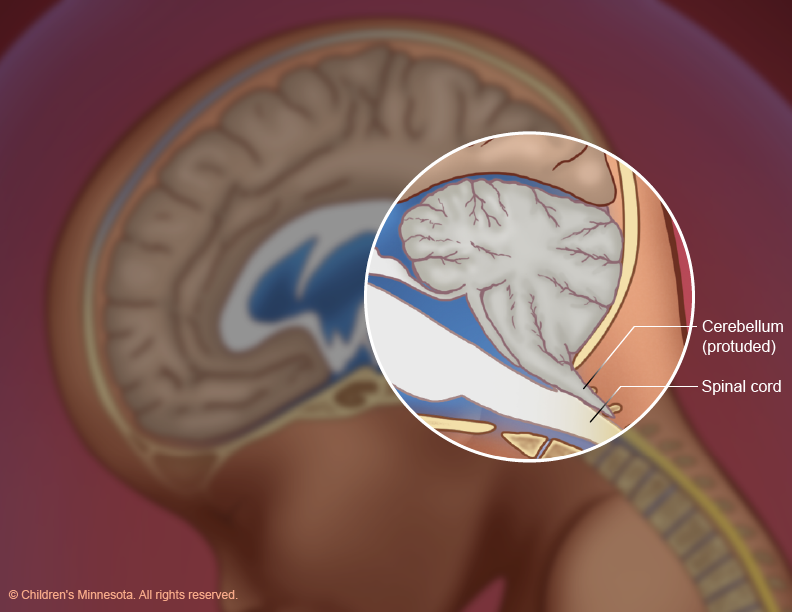
Spina bifida requires surgery to close the spine and stop the injury to the exposed nerves. Due to remarkable medical innovations, myelomeningocele (MMC), the most common form of spina bifida, can be treated prenatally through a surgical procedure known as MMC repair. Until very recently, the only type of prenatal MMC repair was open fetal surgery, a procedure that requires an incision through the mother’s lower abdomen and an additional incision into the uterus to expose the fetal spinal defect. Recent surgical advances now make it possible, however, to sometimes repair myelomeningocele with a less invasive technique: fetoscopic MMC repair, which eliminates the need for a large incision in the uterus. This procedure reduces the risks associated with open fetal surgery, such as rupture of the uterus, and allows the mother the ability to have a vaginal delivery.
Midwest Fetal Care Center is one of just a few medical facilities in North America that offers both open and fetoscopic MMC repair surgery. These complex procedures require a large and skilled clinical team, such as pediatric surgeons, neurosurgeons, maternal fetal medicine specialists, and anesthesiologists, among others.
What happens during prenatal surgery for spina bifida?
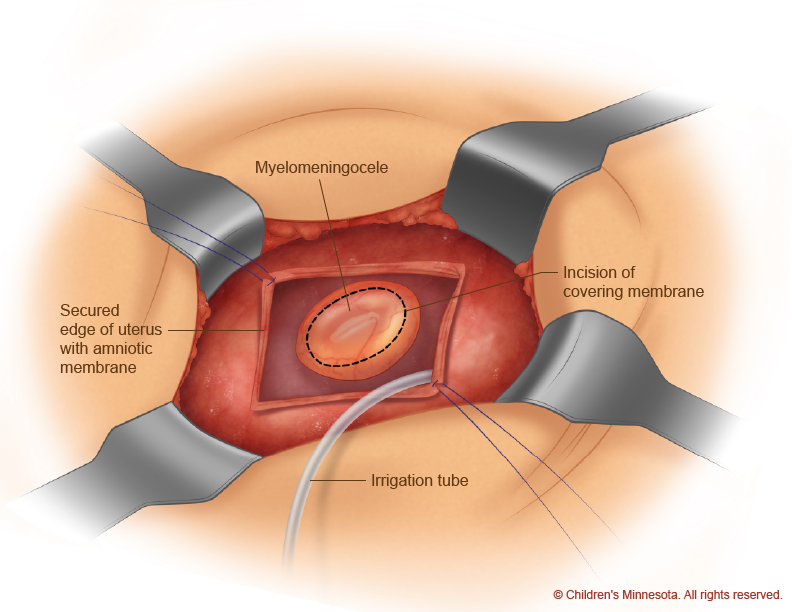
Prenatal MMC repair—whether the surgery is open or fetoscopic—is done before the 26th week of pregnancy. For both procedures, mother and baby are placed under general anesthesia so that both can be operated on simultaneously.
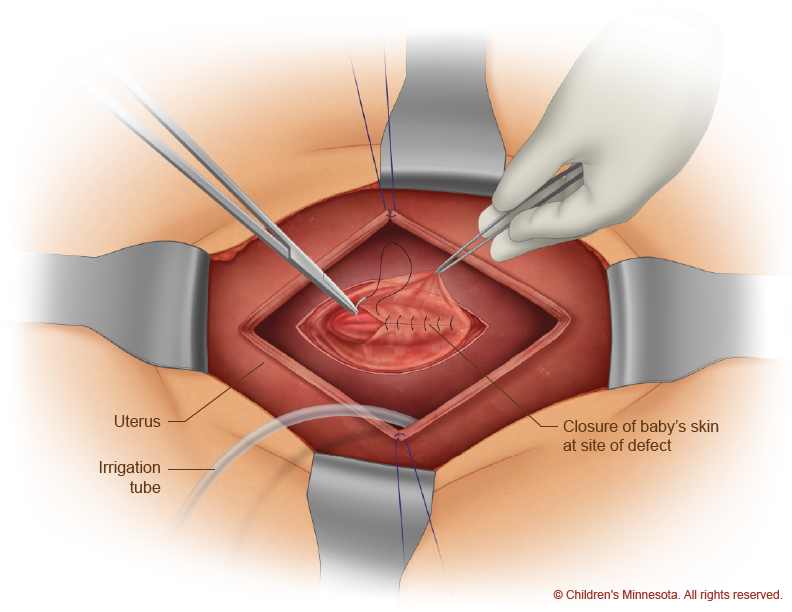
During the open procedure, a horizontal incision is made in the mother’s lower abdomen. Then, using ultrasound imaging, the surgical team makes a safe incision in the uterus, exposing the spinal defect in the unborn baby (Figure 7). With the baby’s back in view, the surgeons remove the sac, if present, and then create a watertight closure of the defect and surrounding tissue (Figure 8).
During the fetoscopic procedure, a similar incision is made in the mother’s abdomen to expose the uterus. Guided by ultrasound images, the surgical team then inserts long, thin tubes—medical devices known as trocars—into the uterus at the location of the gap in the baby’s spine. Using tiny surgical instruments, including miniature cameras, inserted through the trocars, the surgeons then repair the gap in the baby’s spine. This technique eliminates the need for a large incision in the uterus and reduces potential complications for the mother. Once the closure is completed—and watertight—the tubes are removed and the incision in the mother’s abdomen is closed.
In rare cases, the surgical team may switch from a fetoscopic to an open procedure during the surgery in order to ensure the best outcome for both mother and child.