Twin-to-Twin Transfusion Syndrome (TTTS): Early diagnosis and care
Understanding the critical importance of a timely Twin-to-Twin Transfusion Syndrome diagnosis
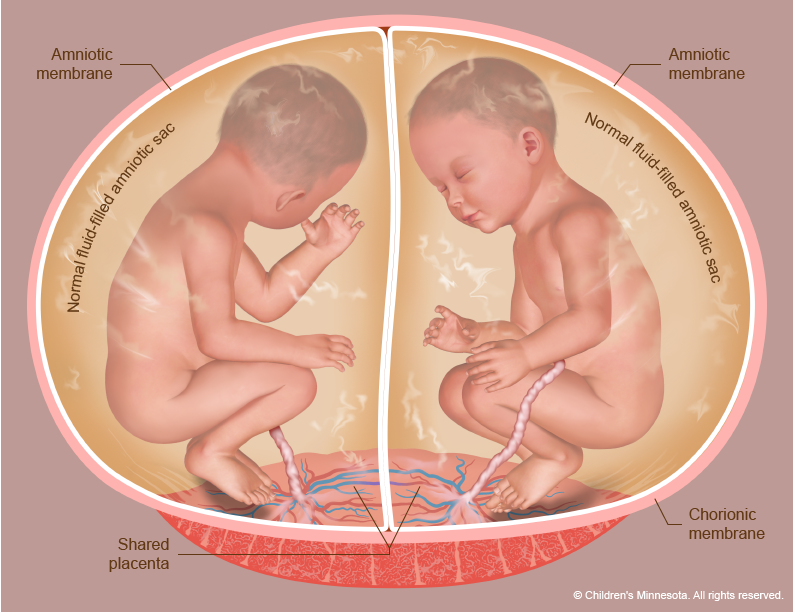
Twin-to-twin transfusion syndrome (TTTS) is a rare yet serious condition that manifests when blood distribution becomes imbalanced between monochorionic twins, referring to pregnancies where two or more genetically identical infants – typically twins – share a single placenta. Among diamniotic twins (those with two separate amniotic sacs), TTTS arises in approximately 10 to 15% of monochorionic pregnancies. The significance of early diagnosis and prompt intervention cannot be overstated in treating TTTS.
People carrying twins with the same placenta should have regular ultrasounds, usually every two weeks starting at 16 weeks, increasing in frequency in the third trimester. Our guide to weekly management and screening of monochorionic gestations gives healthcare providers a week-by-week chart to facilitate early diagnosis and to provide expectant parents with the information they need to make informed decisions about their pregnancy.
What are the risks of Twin-to-Twin Transfusion Syndrome?
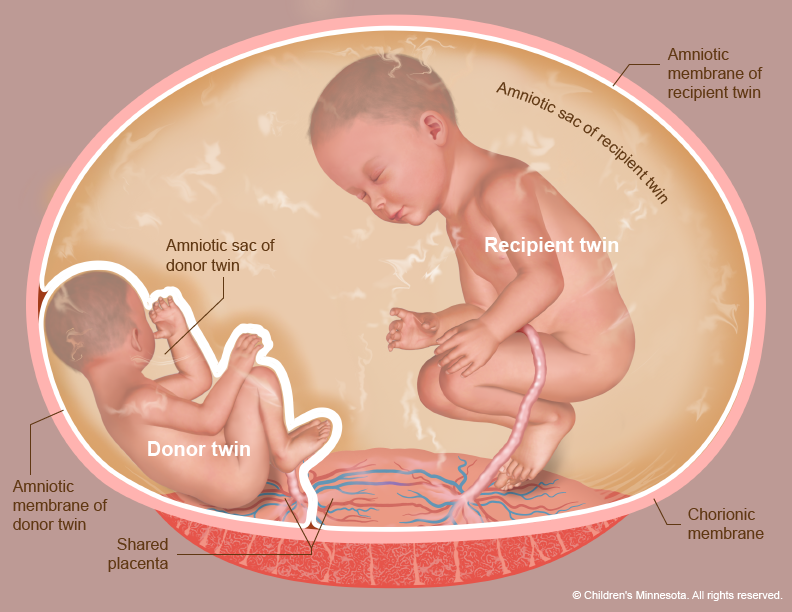
TTTS is a very serious condition that can have life-threatening implications for both unborn twins. One child, known as the donor, can suffer from slow growth, anemia, dehydration, and a decrease in the production of urine, all of which contribute to a lack of amniotic fluid.
For the other twin, known as the recipient, there are a variety of issues that arise such as heart failure, a condition called hydrops which causes excessive swelling, and polycythemia, a condition in which the blood thickens. This twin can also produce an excess of urine, leading to excess levels of amniotic fluid. It is vital that the condition be monitored and treated correctly in order to ensure the health and safety of both twins.
Navigating the path of a Twin-to-Twin Transfusion Syndrome diagnosis
An ultrasound between 10 and 14 weeks can tell if twins share a placenta. TTTS can be seen on ultrasound, usually between 16 and 26 weeks of pregnancy. The scan will show one twin has too much amniotic fluid and the other too little. Impaired blood flow in the umbilical cord may be seen. The mom may see her uterus grow faster than normal. To determine the severity of the condition, we use the Quintero staging system.
Children’s Minnesota management of Twin-to-Twin Transfusion Syndrome
We monitor the fetuses frequently with high-resolution fetal ultrasonography and fetal echocardiography. This testing allows us to measure the amount of amniotic fluid around the fetuses. It also allows us to assess how well blood is flowing within the umbilical cords, as well as within other blood vessels.
Evaluating monochorionic pregnancies and amniotic fluid
The key to TTTS treatment is early diagnosis and intervention. TTTS can develop rapidly – people carrying twins who share a placenta should undergo frequent ultrasounds to evaluate amniotic fluid volumes. Typically, ultrasounds are performed every two weeks, starting at 16 weeks. The frequency of ultrasounds then increases during the third trimester. To see Children’s Minnesota expertise download our guide to weekly management and screening of monochorionic gestations for TTTS.
Our management tools for Twin-to-Twin Transfusion Syndrome include:
- TTTS screening – This screening includes checking amniotic fluid levels, bladder size and function of both fetuses. Doppler sonography of the umbilical artery (UA), fetal middle cerebral artery (MCA), ductus venosus (DV), and umbilical vein (UV) will look for other signs of TTTS or abnormalities.
- Growth ultrasound – Measurements of various body parts are taken to ensure the fetuses are growing normally. The position and movements of the babies are also noted, as well as the position of the placenta and level of amniotic fluid in the womb.
- Level 2 ultrasound (LVL II) – Also known as an anatomy scan, this exam closely looks for abnormalities in the four chambers of the heart, kidneys, bladder, stomach, brain, spine, and genitalia.
- Fetal echocardiogram (echo) – This specialized ultrasound examines the structure and function of the baby’s heart. It helps identify and diagnose congenital heart defects and other abnormalities before birth.
- Antenatal testing – This consists of a biophysical profile (BPP) and a non-stress test (NST) to assess and monitor fetal well-being and placenta function.
Advancing care for Twin-to-twin transfusion syndrome
We are actively involved in research regarding TTTS and collaborate with other advanced fetal care centers in the U.S. and internationally through the North American Fetal Therapy network (NAFTnet) and the International Fetal Medicine Surgery Society (IFMSS). In the last 2 years:
- 95% of procedures resulted in at least one twin surviving
- 73% of procedures resulted in both twins surviving
See full outcomes data
Meet The Kid Experts who specialize in Twin-to-Twin Transfusion Syndrome
The Midwest Fetal Care Center (MWFCC), a collaboration between Allina Health and Children’s Minnesota, brings together a multi-disciplinary team of highly trained maternal-fetal medicine experts from Allina Health and pediatric and neonatal specialists from Children’s Minnesota. Meet our TTTS kid experts:
Clifton Brock, MD
Saul Snowise, MD
Contact us
Need a referral or more information? You or your provider can reach the Midwest Fetal Care Center at 855-693-3825.