Who will be on my care team?
At Midwest Fetal Care Center, a collaboration between Children’s Minnesota and Allina Health, we specialize in individual attention that starts with you having your own personal care coordinator to help you navigate the complex process of caring for your babies. We use a comprehensive team approach to twin to twin transfusion syndrome treatment. That way, you are assured of getting the best possible information by some of the most experienced physicians in the country. For TTTS, your care team will include a maternal-fetal specialist, a fetal interventionist, a pediatric cardiologist, a neonatologist, a nurse specialist care coordinator, a fetal care clinical social worker and several other technical specialists. This entire team will follow you and your babies closely through the evaluation process, and the team will be responsible for designing and carrying out your complete care plan.
Meet the team
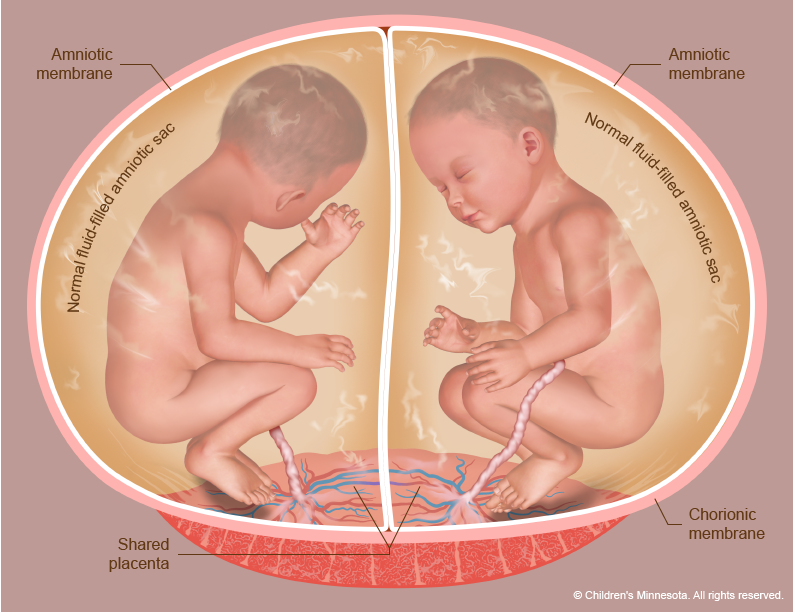
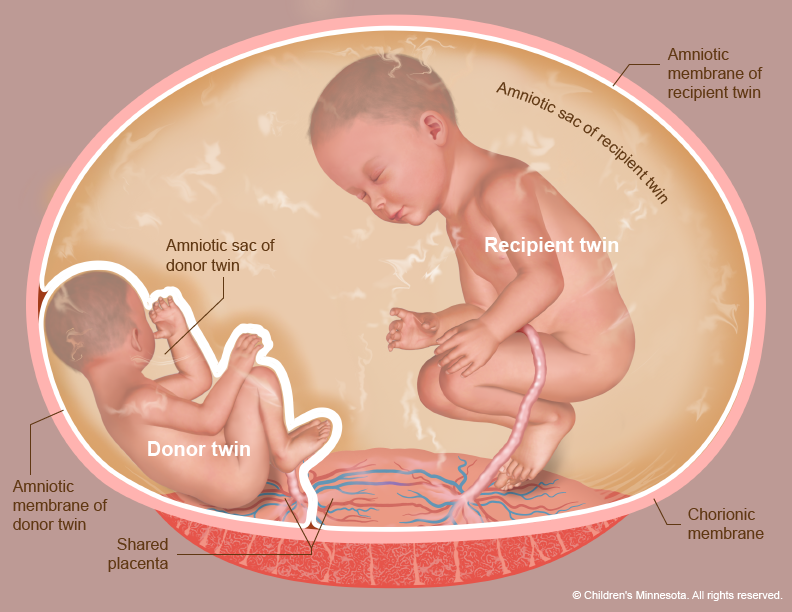
What causes twin to twin transfusion syndrome (TTTS)?
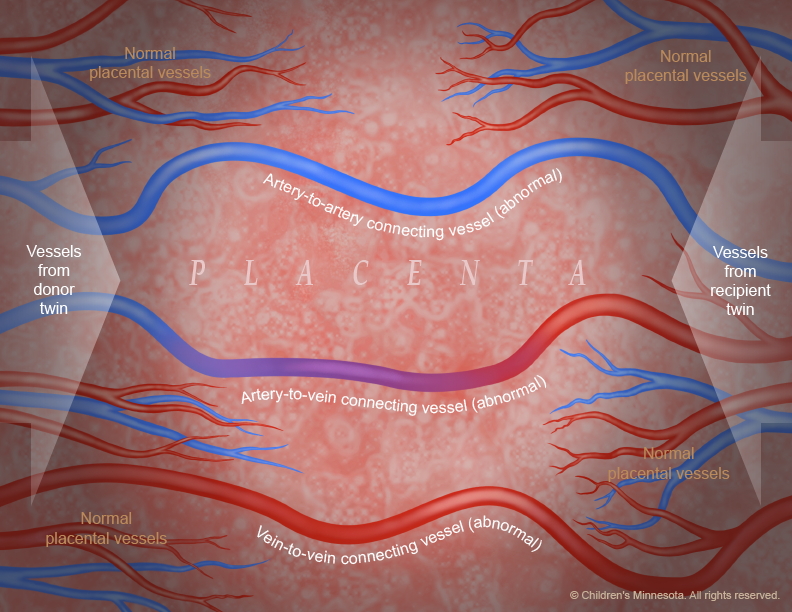
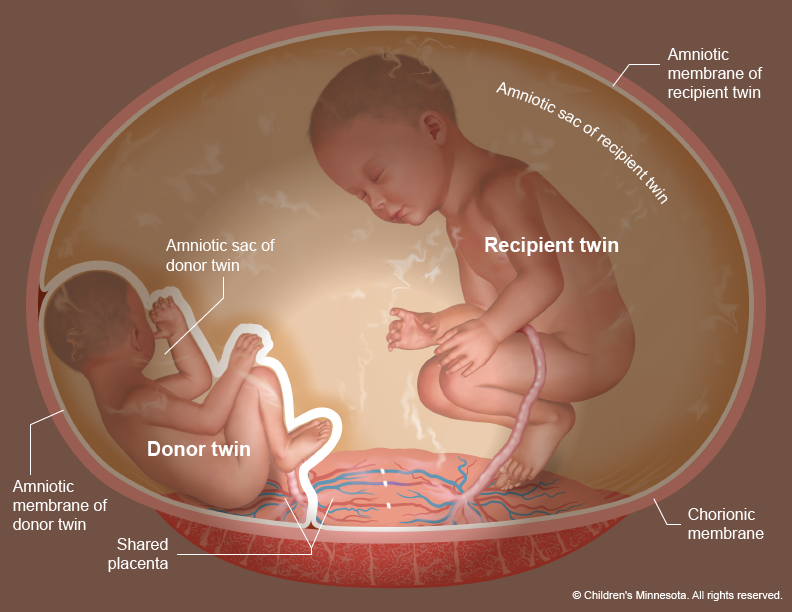
The placenta is a very active organ and provides babies with oxygen and nutrients during pregnancy. It grows along with the babies. Sometimes, for reasons that are not well understood, the normal flow of blood in the placenta’s blood vessels develops an abnormal pattern. When unborn babies share a placenta, the result can be an imbalance in blood circulation, with one baby receiving too much blood through the umbilical cord and the other receiving too little. It is this imbalance that leads to TTTS.
How is twin to twin transfusion syndrome (TTTS) diagnosed?
A twin to twin transfusion syndrome diagnosis is confirmed by ultrasound. The condition becomes evident when the ultrasound images show that one child has extra amniotic fluid and the other child has significantly decreased amounts. Abnormalities in the blood-flow patterns in the umbilical cord may also be found. In addition, the mother may experience a rapid enlargement of her uterus — more quickly than is expected during pregnancy.
Because TTTS can develop rapidly, women carrying twins who share a placenta should undergo frequent ultrasounds to evaluate amniotic fluid volumes. Typically, ultrasounds are performed every two weeks, starting at 16 weeks. The frequency of ultrasounds then increases during the third trimester.
Learn more about our guide for weekly management and screening of monochorionic gestations for TTTS.
What is Quintero staging, and how is it used for babies with twin to twin transfusion syndrome (TTTS)?
When TTTS is diagnosed, a staging system is used to classify the severity of the condition. This system — known as the Quintero staging system — helps to determine whether an intervention is needed and which treatment option(s) might be most appropriate. Here is an explanation of twin to twin transfusion syndrome stages:
Stage I: The ultrasound shows an imbalance of amniotic fluid around the twins, but the donor twin’s bladder is still visible. The visibility of the bladder indicates the donor baby is receiving enough nutrients and fluid through the blood to produce urine.
Stage II: The ultrasound shows an imbalance of amniotic fluid around the twins, but the donor twin’s bladder is not visible. This finding indicates the bladder is empty — a sign that the baby has stopped making urine.
Stage III: In addition to the Stage I and II indicators, the ultrasound shows significant abnormalities in the flow of blood within the twins’ umbilical cords.
Stage IV: In addition to the Stages I-III indicators, the recipient twin shows signs of heart failure (hydrops fetalis, or extra fluid within the baby).
How is twin to twin transfusion syndrome (TTTS) managed before birth?
Our prenatal management of babies with TTTS centers on monitoring the babies frequently with high-resolution fetal ultrasonography and fetal echocardiography. This testing allows us to measure the amount of amniotic fluid around your babies. It also allows us to assess how well blood is flowing within your babies’ umbilical cords, as well as within other blood vessels.
What is high-resolution fetal ultrasonography?
High-resolution fetal ultrasonography is a non-invasive test performed by one of our ultrasound specialists. The test uses reflected sound waves to create images of your babies within the womb. We will use ultrasonography to follow the development of your babies’ internal organs and overall growth, as well as the volume of amniotic fluid that surrounds them throughout the pregnancy.
What is fetal echocardiogram?
Fetal echocardiography (“echo” for short) is performed at our center by a pediatric cardiologist (a physician who specializes in fetal heart abnormalities). This non-invasive, high-resolution ultrasound procedure looks specifically at how your babies’ hearts are structured and function while in the womb.
How can twin to twin transfusion syndrome (TTTS) be treated before birth?
The key to twin to twin transfusion syndrome treatment is early diagnosis and intervention. What treatment option will be best for your babies will depend on the stage of the TTTS and your babies’ gestational age at diagnosis. Several options are available, including the following:
- Expectant management: This involves continued close ultrasound surveillance throughout the pregnancy. We currently recommend expectant management for most Stage 1 TTTS.
- Amnioreduction: This is a procedure that is used to remove excess fluid that has accumulated in the amniotic sac of the recipient twin. The procedure is similar to that of amniocentesis, with the doctor using “real-time” ultrasound images to guide a long, very fine needle into the uterus to withdraw the fluid. We may recommend this intervention for Stage 1 TTTS or when the TTTS is diagnosed later in the pregnancy and fetoscopic laser photocoagulation (see below) is no longer an option.
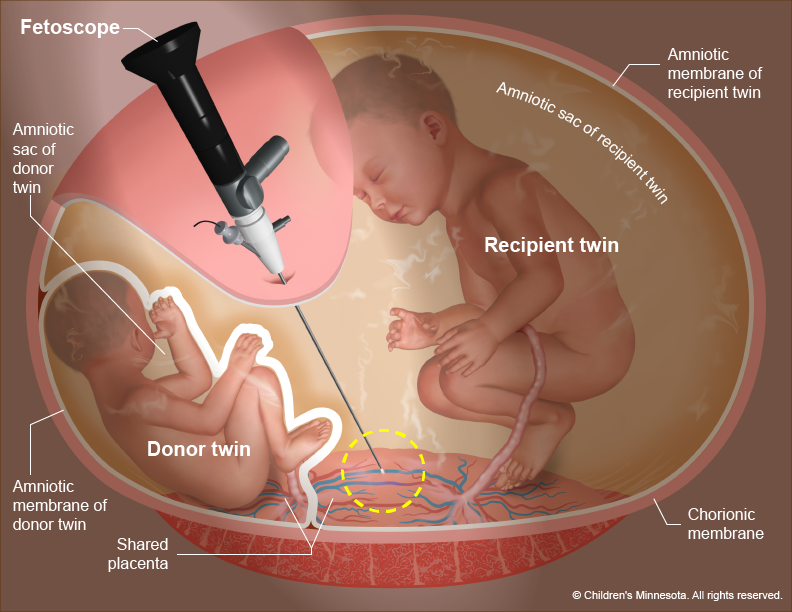
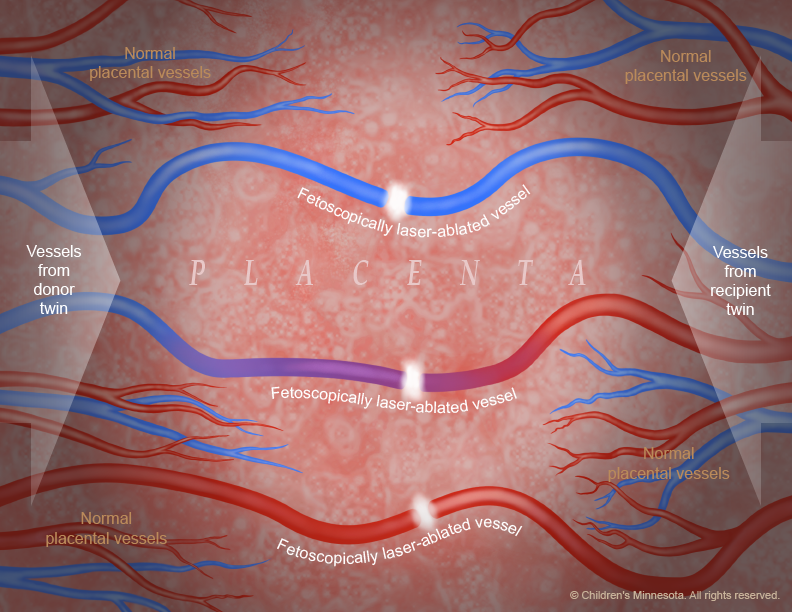
- Fetoscopic laser photocoagulation: This minimally invasive surgery uses a laser to ablate (seal) blood vessels that are contributing to the abnormal flow of blood to the babies (Figures 3-5). Many studies have demonstrated that this procedure for the treatment of twin to twin transfusion syndrome is the most effective therapy for babies with advanced TTTS.
- Delivery: If TTTS is discovered later in the pregnancy, delivery of the babies may be the best option.