Cortisol Replacement Treatment
Your child has been diagnosed with a disorder where he or she is unable to make enough cortisol. Cortisol deficiency can be threatening to life and health. Once the diagnosis of deficiency is made, treatment is necessary. When cortisol is made by the body, the levels can be variable throughout the day. In general, the body makes the most in the early hours of the morning and the least in the late afternoon. These levels also may fluctuate depending upon illness stress fever or injury. Understanding the reasons why the body's cortisol levels may vary, are important for proper replacement.
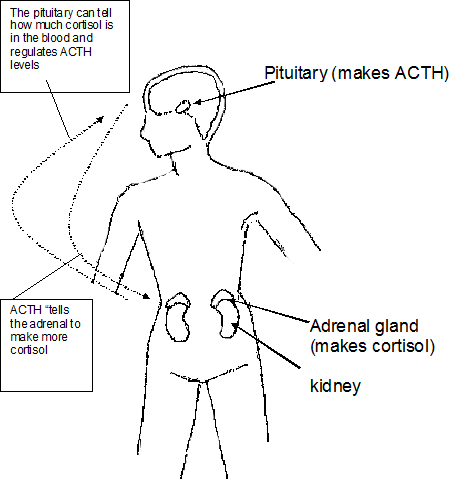
Cortisol is a hormone made by the body, with the main function of helping the body respond to stress. It is one of many hormones produced by the adrenal glands. Like many of our endocrine glands, the adrenal glands are controlled by the pituitary gland. The pituitary gland is situated in the brain. One of the hormones the pituitary gland makes, ACTH or adrenocorticotropic hormone, controls the adrenal gland. If larger amounts of cortisol or other adrenal hormones are needed, the ACTH level goes up. If too much cortisol is either given or made by the body, the ACTH level will go down. The pituitary gland, in turn, is controlled by another part of the brain called the hypothalamus. Cortisol production can be affected when there are problems with any part of this system: the hypothalamus, the pituitary, or the adrenal glands.
Low ACTH
- The pituitary (brain) isn’t making enough ACTH, adrenals are not getting stimulation to make cortisol.
- The adrenal glands do not know that they need to make cortisol, so not enough is made.
High ACTH
- The pituitary (brain) is working harder than normal to get the adrenals to make cortisol.
- The adrenal glands are not working well and can’t make enough cortisol.
Development of cortisol deficiency
A problem in any of the steps by which cortisol secretion is regulated can lead to a deficiency of cortisol.
There may be problems with the brain, especially the pituitary gland. If it does not work, ACTH cannot be made. When this happens, the adrenal glands are not stimulated and do not produce their hormones.
When this happens, the diagnosis is hypopituitarism.
Other times, the adrenal gland may not work properly. Problems that can cause this may be present from birth, for example, congenital adrenal hyperplasia. If the problem develops after birth, it can be from infection, autoimmune disease, or injury. This is called adrenal failure, or sometimes Addison’s disease.
For either of these problems, the end result is that the adrenal glands to not make enough cortisol, and replacement treatment must be taken. For these problems, the need for hydrocortisone replacement is lifelong. It is very rare for a child to outgrow the need for medication. Occasionally this may happen if the adrenal failure is secondary to injury or surgery.
Never stop your child's hydrocortisone unless instructed by your doctor.
Cortisol’s actions in the body
Cortisol is essential for her life and health. If there is a mild deficiency, generally people feel ill, lose weight and have loss of appetite. A person may die from a severe deficiency.
Effects of cortisol:
- Maintain energy balance
- Help the body manage stress
- Help the body manage fluids such as sodium and potassium (blood salts)
- Help maintain blood pressure
- Help maintain blood sugar levels
- Help manage the body’s immune response
Other effects of cortisol:
The cortisol doses or amounts that are used to replace a deficiency are called physiologic. This means your doctor is trying to give the exact dose the body would normally be making. When dosed this way, there are no bad side effects from the hormone.
If a person has certain other medical problems such as asthma, arthritis, or certain types of cancer, very large doses of cortisol or similar medications (prednisone or dexamethasone) may be given. In very large doses, cortisol (steroids) often has side effects such as weight gain, poor growth, high blood sugars and changes in the body's immune system. The doses required to cause these effects are many times the “physiologic” (maintenance or daily) replacement dose.
When your child’s doctor prescribes hydrocortisone to replace their cortisol deficiency, he or she pays special attention to give doses that are considered physiologic. Physiologic doses are those required every day to maintain energy balance, blood pressure and blood sugar levels.
Getting the right dose
Initially, a when your child starts taking this hormone, his or her doctor will use a calculation based on height and weight to come up with the right dose. In addition to height and weight, growth and laboratory tests are often used to be certain the dose is right.
Types of cortisol replacement
There are several different formulations of medication that can be used to treat cortisol deficiency. In growing children, the most common is hydrocortisone. Other medications that are sometimes used are dexamethasone (decadron), or prednisone. For emergencies, injectable forms are used, which are discussed in the following pages. The different medications are very different in their strengths and length of action, so it is very important not to substitute one for another without specific instructions from your child’s doctor. Since hydrocortisone (Cortef) is used most often, it will be referred to in this guide.
Missed doses
It is very important that your child gets his or her doses within 2-3 hours of the prescribed time. If you find that you are missing doses or forgetting frequently, try to determine why and plan a system to prevent it. Plans that may help include:
- leave the medication visible on the countertop so it is seen when you pass through the house
- use a pill reminder container
- try to link giving the dose with certain regular events in your child’s daily routine such as meal or snack times
- use a calendar with stickers or check marks to keep track of doses taken
What you should do if your child misses a dose or forgets a dose will be determined by the doctor. This will depend on your child's medical condition. Your child may be instructed to double the dose if it has been 4 hours or more than 2 doses are missed.
Treatment during illness
Normally when a person is ill, has had an injury, or fever, the body makes more cortisol. This helps the body handle the stress of the injury, illness or fever. When a person with cortisol deficiency takes treatment, he or she needs to learn which situations will require extra or “stress” dosing.
The usual stress dose treatment is 3 times the child's usual dose.
Stress doses are given when the child is:
- ill with a fever
- throwing up
- having surgery or dental procedures
- severely injured such as a broken bone, head injury, concussion, car accident or bike accident resulting in injury
- sick with a viral illness that would normally keep him or her home from school including those with the vomiting and diarrhea
If you are in doubt about whether or not to give your child a stress dose, you can call your doctor, or if you are not able, you can give the stress dose and discuss this with your doctor afterward. You will not harm your child by giving a stress dose unnecessarily. Often parents recognize physical signs that their child will show when they need a stress dose. Watch your child carefully when he or she is ill so you can learn these signs.
Stress dosing by injection
If your child is throwing up and cannot take the hydrocortisone by mouth, he or she will need another form of medication as an injection. The dose of this medication (Solu-Cortef) will be determined based on your child's height and weight. In general, the injection of Solu-Cortef lasts about 6 hours.
Sometimes a child will become ill rapidly and will need an injection of the Solu-Cortef as the first treatment.
Signs and symptoms include:
- confusion
- fever
- dazed
- throwing up or nausea
- dizzy
- unusually tired
- listless
- unusually weak or lethargic
- headache
- unconscious
Even though the Solu-Cortef is not needed often, and sometimes never in some children, you need to have this available in case of an emergency. If you are unsure in an emergency situation, you should give the injection. You cannot hurt your child by giving an unnecessary dose.
If you need to give the Solu-Cortef by injection, your child should be seen by his or her doctor or in the emergency department. The intramuscular injection lasts about 6 hours once it is given, so a plan needs to be made regarding what to do for continuing treatment if your child is still sick after the initial injection is given. If your child is unconscious, you should give the injection and call 911.
How long to continue the stress doses
Go back to your child's usual dose when:
- your child's fever has been gone for 12 to 24 hours
- he or she is stable after an injury or medical problem
For some conditions, the stress doses may need to be tapered. Your child's doctor will give instructions if this is necessary.
How to give an injection of Solu-Cortef
Getting the injection ready
- Wash your hands.
- Get your equipment ready:
- syringe with needle
- alcohol pad (or cotton ball and rubbing alcohol)
- Solu-Cortef “Act-o-vial” - Push down on the top of the Act-o-vial to release the cork.
- Shake gently to mix the contents.
- Take the top off the Act-o-vial. Wipe the rubber stopper with an alcohol pad. Take the cap off the syringe and insert the needle through the middle of the stopper. Stop when you can see just the tip of the needle in the Act-o-vial.
- Turn the vial upside down and pull back the plunger on the syringe until you have the right amount of Solu-Cortef in the syringe. Keep the tip of the needle below the surface of the liquid to avoid getting air in the syringe.
Before you remove the needle from the stopper, it is ok to push the plunger up to get rid of air bubbles and to re-draw the correct amount of medicine.
Once you pull the needle out of the vial, replace the cap on the needle until you are ready to use it.
Giving the injection (shot)
- Pick the spot you will inject. Usually, this is the front of the thigh (middle, top part of a child’s leg). Clean the area with the alcohol pad.
- Take the cap off the needle and hold the syringe like a pencil or dart.
- Hold the skin and muscle between your thumb and first finger, pushing down slightly.
- Put the needle in at a right angle. Try to put it in quickly.
- Check to be sure the needle is not in a blood vessel by pulling gently up on the plunger while holding the needle in place. This can be done with your thumb or other hand.
If no blood appears, push the plunger down all the way to give the dose.
If blood appears in the syringe, remove the needle without giving the injection and start over. If this is your only dose, you must give it. Pull the needle back about ¼ inch and give the injection. - After you have given the injection, pull the needle out quickly and put a cotton ball or gauze over the site if there is any oozing.
Medical identification
Any person, child or adult, with adrenal insufficiency needs to wear a medical identification necklace or bracelet. It should say something like, "adrenal insufficient, takes hydrocortisone, cortisol dependent". This will protect your child if something happens when you are not present. Medical personnel are trained to look for medical identification when responding to emergencies.
As your child gets older and spends more time with his or her friends and learns to drive a car, this identification is very important.
Sports/Camps/Trips
Anyone caring for your child should be informed of the need for cortisol replacement. This includes doctors, school nurse, babysitter or camp counselor. Sports and any activity that takes your child away from home overnight or longer will require enough hydrocortisone for stress coverage as well as a vial of injectable hydrocortisone in the case of an emergency. There also should be a plan designating a person who can give a shot if needed.
Questions?
This is not specific to your child but provides general information. If you have any questions, please ask your doctor, nurse or other health care team members working with your family.
This page is not specific to your child, but provides general information on the topic above. If you have any questions, please call your clinic. For more reading material about this and other health topics, please call or visit Children's Minnesota Family Resource Center library, or visit www.childrensmn.org/educationmaterials.
© 2024 Children's Minnesota
