Pneumothorax (Spontaneous)
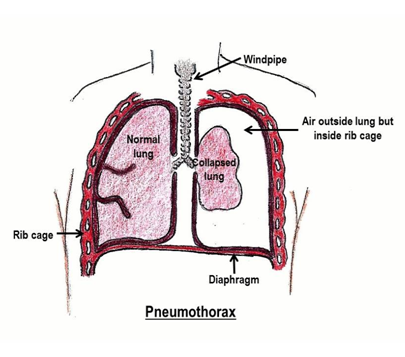
A pneumothorax (air leak) is an abnormal collection of air in the space between the lung and chest wall. It can occur in children with no other lung problems because of a small area of weakness in the lung. This area can open, allowing air into the space outside the lung. This air pushes on the lung and can collapse it.
What are the signs and symptoms?
Symptoms are more likely to develop at rest than during physical activity and may include:
- acute chest pain that improves over time
- shortness of breath
- back and shoulder pain
Sometimes the heart is affected. This is called a tension pneumothorax. Signs of this are:
- Walking, even standing with breathing difficulty
- Breathing difficulty and chest pain with anxiety
- Gasping with shallow breathing
- White, grey, or blue skin color with or without sweating
How is pneumothorax diagnosed?
Tests are ordered to diagnose pneumothorax.
- A chest X-ray shows if pneumothorax is present. This allows the doctor to estimate the size of the pneumothorax.
- A computed tomography scan (CT scan) of the chest is rarely required. Sometimes it is performed to make the diagnosis and look for rare complications.
How is it treated?
- Observation and oxygen may be recommended if the pneumothorax is small in size and your child does not have a breathing problem at rest. This may or may not require your child to stay in the hospital. If admitted, the expected length of stay ranges from ½ day to 3 days but full expansion of the lung may take up to 1 month.
- Needle aspiration may be recommended. A small needle is inserted through the chest wall. A syringe is connected to the needle and the air is pulled out. If the air does not re-collect after 24 hours, your child will be discharged home. If air rapidly returns to the space outside the lung, another procedure will be necessary.
- Chest tube insertion. In this treatment, a tube is inserted between the ribs and into the space around the lungs to drain the air. It is connected to a one-way valve in a bedside container that allows air to escape but not re-enter. The tube is left in place until air is no longer seen exiting into the container.
- Heimlich valve is a one-way valve that is attached to the chest tube allowing air to leak out of the chest but barring air from entering. This device is portable and patients can be discharged with a Heimlich valve with follow-up within 24 hours of discharge. Heimlich valves are usually reserved for adults with pneumothorax.
-
Surgery is considered if:
- The pneumothorax is large or has created tension.
- A pneumothorax treated with a chest tube is unsuccessful and air continues to leak for more than 3 days.
- The patient has had more than one pneumothorax.
- The patient had a pneumothorax occur on both sides at the same time.
This surgery is called a VATs procedure (Video-Assisted Thoracoscopic surgery). Several small incisions are made in the chest wall. The areas of lung weakness are removed and the outer surface of the lung is stuck to the inside surface of the chest wall to keep the lung from collapsing again.
What else do I need to know?
- Usually, a pneumothorax only involves one lung but it can involve both sides.
- There is a chance that pneumothorax can occur again. Your doctor will go over the risks associated with each treatment option.
- Most repeat pneumothorax occur within 2 years of the first event.
- Precautions to take:
- No scuba diving – EVER.
- No airline travel for 4 weeks.
- No contact sports for 4-6 weeks.
Examples include: football, lacrosse, rugby, hockey, wrestling - No heavy exercise at sea level for 4-6 weeks.
Examples include: weight lifting, running, swimming. - No exercise at altitude (>8,000 feet) for 4-6 weeks.
Examples include: skiing, mountain climbing - An alternative to aerobic work is to challenge the athlete with a focus on other aspects of their sport: technique, competitiveness, teamwork, and leadership. Video review of a young person’s performance particularly with a coach will only enhance performance when he/she returns to the activity.
How should I care for my child at home?
- Watch your child for any returning symptoms of a collapsed lung including shortness of breath, chest pain, or difficulty with exercise.
- Give your child any pain relief or other medications as directed by the doctor.
- Leave the bandage in place for 72 hours. If there is any drainage or the wound still looks open when you remove the bandage, replace it with gauze and tape as you were shown.
- After 72 hours, your child may shower with a bandage in place, but should not take a bath or soak in water until the surgical wound is completely healed over and does not need a bandage.
- Make sure your child returns for all follow-up visits.
Call your doctor if your child has:
- Redness, pus, or swelling at the surgical wound site.
- A temperature of 101°F (38.3°C) or higher.
- Pain that is not improving with pain medication.
Call 911 if your child:
- Has shortness of breath, especially if it comes on suddenly.
- Has worsening chest pain.
- Is pale, dizzy, or weak.
Questions?
This is not specific to your child but provides general information. If you have any questions, please call your clinic.
Reviewed by Kuracheck 2/2017
This page is not specific to your child, but provides general information on the topic above. If you have any questions, please call your clinic. For more reading material about this and other health topics, please call or visit Children's Minnesota Family Resource Center library, or visit www.childrensmn.org/educationmaterials.
© 2024 Children's Minnesota
