Lichen sclerosus
What is lichen sclerosus?
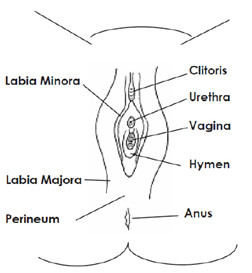
Lichen sclerosus (LIKE-in skler-O-sus) is a skin disorder that affects the vulva (the skin surrounding the vagina). It can happen at any age. It is most common in adults who stopped having their periods (post-menopausal), but can also happen in younger children and teens. In children, it usually appears before menstrual periods start. For some patients, it will go away with periods, but not always, so it is important to follow up with your doctor as directed.
What are the symtoms?
The most common symptoms are itching, irritation, or pain in the skin around the vagina. Sometimes there can be small breaks or “cuts” in the skin that are painful. The way the skin of the vulva looks may also change. Often, the skin looks lighter than the areas around it and may also look thinner, more fragile, or crinkly. Other times, patients may not have any symptoms that they notice.
Often, the lightened area looks like a hourglass or figure of 8 shape around the vulva and anus (where poop comes out). Because the skin is thin, it tears easily, causing pain and bleeding. Bleeding under the skin can cause bright red or purple marks or “blood blisters.” It can also cause pain or burning with peeing or pooping. Women may choose to avoid sex, tight clothing, tampons, riding bikes or horses, and other common activities that involve pressure or friction in the vaginal area.
If lichen sclerosus is not treated or if patients do not follow up as directed, they might get scarring in the vaginal area. The result may be that the inner lips of the vulva shrink and disappear, the clitoris becomes covered with scar tissue, and/or the opening of the vagina may narrow.
If lichen sclerosus is present around the anus it can contribute to constipation (makes it hard to poop). In addition to using the ointment, treatment of constipation is important.
What causes lichen sclerosus?
The cause of lichen sclerosus is not completely understood, but an overactive immune system may play a role. There may be a genetic tendency toward the disease. It is not normally due to an infection or trauma.
How is lichen sclerosus diagnosed?
Lichen sclerosus can be diagnosed in the office by looking at the skin. Sometimes your doctor might need to check a sample of your skin (biopsy) to confirm the diagnosis. A biopsy is usually not necessary.
Genital area of a young patient
How is lichen sclerosus treated?
Lichen sclerosus is a chronic condition that needs ongoing treatment – even if there are no symptoms. Continuing treatment will help prevent symptoms and scarring.
Prescription medicines are required to treat lichen sclerosus. The first treatment of choice is a strong steroid ointment (Clobetasol). Patients use the ointment for about 6 weeks and then their doctor will recheck the area. If things are getting better, the doctor may tell them to use the ointment less often or change to a different ointment. If things are still irritated, patients may continue to use the Clobetasol ointment another 6 weeks. It is important to follow up as scheduled so your doctor can make these changes. Use of these ointments can stop the symptoms (itching and bleeding), help the skin to heal and prevent scarring. Even after the symptoms go away, the medicine should be continued according to your clinicians instructions to prevent scarring and prevent the symptoms from coming back.
Some girls may require lifelong treatment. Lichen sclerosus symptoms may or may not disappear at puberty. Scarring and changes in skin color may not go away even after the symptoms of pain and itching have gone away.
Vulvar care
- Teach good hygiene
- Wash hands before and after using the bathroom.
- Wipe from front to back after peeing or pooping.
- Pee with knees spread apart while leaning forward and stay seated on the toilet until finished urinating to allow all the pee to come out. For smaller children, it also might be helpful for them to sit backwards on the toilet (facing the tank) so they feel more supported.
- Take a plain water bath (not a shower) every day. Soak in a frog-leg position in a tub of plain, warm (not hot) water for 10 minutes daily.
- Avoid constipation. If your child is not having a soft, daily bowel movement they may have constipation and require treatment. Discuss this with your doctor.
- Avoid irritation
-
Wear cotton underwear during the day and avoid wearing underwear at night.
- Avoid harsh laundry detergents and make sure underwear is rinsed thoroughly. Avoid fabric softeners and dryer sheets.
- Do not use bubble bath or add anything else to bath water unless prescribed by your doctor.
- Avoid using soap in the sensitive vaginal area; this area can be cleansed with a soft cloth and water alone. Use a mild, hypoallergenic bar cleanser, such as unscented Dove® on the rest of the body. Avoid deodorant soaps.
- Make sure all soaps are washed off after bathing, and do not allow soaps or shampoo to float around in the bathtub. Your child should stand in the tub when using soaps instead of sitting in the soapy water.
- Avoid tight jeans or pants, and tights.
- Avoid sitting in a wet bathing suit after swimming – rinse chlorine off of the vulvar area after swimming and change as soon as possible into dry clothing.
- You can try applying a protective ointment, like Vaseline (petroleum jelly), if recommended by your provider.
Questions?
This is not specific to your child but provides general information. If you have any questions, please call the clinic.
Reviewesd by GYN 7/2022
This page is not specific to your child, but provides general information on the topic above. If you have any questions, please call your clinic. For more reading material about this and other health topics, please call or visit Children's Minnesota Family Resource Center library, or visit www.childrensmn.org/educationmaterials.
© 2024 Children's Minnesota
