Nasogastric (NG) Tube Feeding
Article Translations: (Spanish) (Somali)
What is a nasogastric tube feeding?
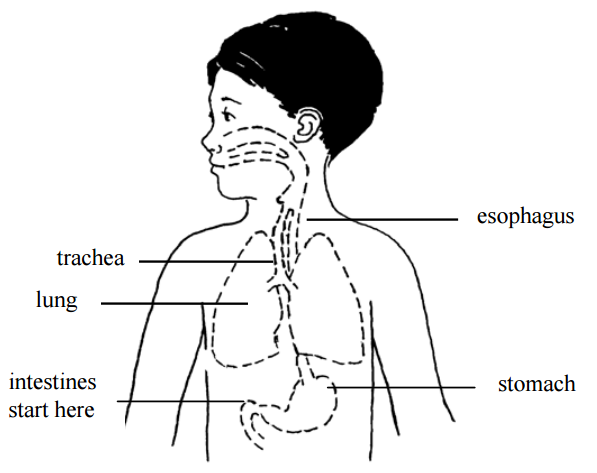
A nasogastric (NG) tube is a small tube that goes into the stomach through the nose. Breast milk, formula, or liquid food is given through the tube directly into the stomach, giving your child extra calories. Feeding this way helps your child get enough nutrition to grow, develop, recover from illness, play, and learn.
Tube feeding can be done for children of any age. Some children will depend on tube feeding only until they are able to eat by mouth. Using the gastrointestinal (GI) tract for feeding keeps it healthy and working normally.
Other children can continue to eat as usual, and also get tube feedings for extra calories.
There are several ways to give NG feeding. The type of tube, how often it needs to be changed, type and amount of formula, and length of feeding time will be decided by the doctor and dietitian, depending on your child's needs.
Follow only the checked instructions in this sheet.
Your child's special instructions:Type and size of feeding tube: ___ Change the feeding tube every: ___ Do not change the feeding tube yourself. What to feed: Amount to feed: How often to feed: Method: ___ bolus ___ continuous Type of pump: Rate of feeding: Flush the feeding tube at the end of each feeding with ml of warm water. Other: Measurement: Marking at nostril: _____cm Nostril to beginning of the hub: _____cm Care of feeding bag and tubing:___ Change every day. If the bag and tubing do not clean easily, try using a solution made of equal amounts of white vinegar and cool water (for example 1 cup vinegar with 1 cup water). Rinse well and store in refrigerator. Throw away the feeding bag and tubing after 1 week; sooner if you cannot get it clean or if it begins to leak. |
Definitions
|
aspiration |
getting fluid (stomach contents for formula) into the lungs, which can cause trouble breathing |
|
bolus |
feeding over a short time |
|
continuous |
feeding over an extended time at a slower rate |
|
GI tract |
the esophagus, stomach, and intestines |
|
lubricant |
water-soluble substance such as K-Y® jelly, used to help the tube slip in more easily - do not use Vaseline® |
___ Inserting the feeding tube
It takes time and practice to learn how to insert the tube, so be patient with yourself. Do this by yourself only after you have done it successfully with the nurse present.
Get ready:
- Wash your hands.
- Gather supplies:
- feeding tube
- tape measure
- With your fingers, find your child's sternum (breastbone). Gently feel the bone in the center of the chest, and then find its bottom edge. It will be below nipple level, and you will feel the bottom of the rib cage curving away to each side.
- Now imagine a spot on your child's belly that is midway between the belly button and the bottom edge of the breastbone. Keep that spot in mind.
- Using a tape measure, measure from the tip of your child's nose to the bottom of the earlobe, then down to that spot midway between belly button and breastbone edge. Write that number down: we will call it "your child's measurement." Measurement:
In this picture, the child's measurement is 12 inches (3 inches from nose to ear, plus another 9 inches down).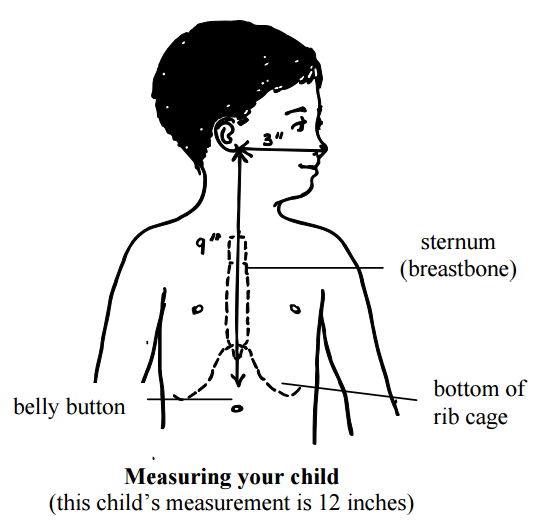
- Now, from the tip of the tube, measure the distance of your child's measurement (in the pictured example this would be 12 inches). Mark that spot on the tube using a permanent marker. Now you are ready to insert the feeding tube.
- Now, measure from the mark you made to the beginning of the hub. That is the Extra Tube Length.
Insert the tube:
- Wash your hands.
- Gather equipment:
- feeding tube
- formula
- gauze if needed
- water for lubrication or other lubricant
- pH testing strips
- syringe, size:
- tape, type:
- water for rinsing if needed
- Position the child.
___ Swaddle an infant (wrap with the arms secured in a blanket). Put your infant on their back, either in an infant seat or on a bed, with the head raised.
___ Older children should be placed in a comfortable position, and may be held by an adult if they wish. Some children may vomit when the tube is put in. Be sure the child can be turned easily if this happens. - Lubricate the tube with water or put a small amount of lubricant on the end of the tube if you have been taught to do so. Most tubes have a coating that is activated with water, making the tube easier to slide in.
- Insert the tube into the nostril, pushing the tube gently down until the mark on the tube is at the tip of the nose. Older children can drink or swallow to help the tube go down. Infants may suck on a pacifier or your fingers during tube insertion. This can be uncomfortable for your child and it is normal for them to cough or sneeze while the tube is being inserted. It may be best to have someone help you.
After the tube is inserted, remove the tube right away if:
- coughing
- gagging
- sneezing
- vomiting
- wheezing
- changing color
- cannot catch a breath
- change in respiratory rate
- change in oxygen needs
- decrease in pulse oximeter readings
- increased restlessness
- unexplained irritability, discomfort, or abdominal pain
- or you see the tube coming out of the mouth
- Cuddle and comfort your child for a few minutes, and try again.
- Once the tube is in place, secure it with tape as shown by the nurse.
- Check the tube placement (see below).
Checking the tube placement
To prevent aspiration, you must check the tube placement before each feeding, to be sure it has not moved. The stomach should be as empty as possible when checking for placement, so plan each placement check before medicine or feedings.
- Look at your child. Is your child comfortable and breathing normally? If your child appears distressed, gagging, sneezing, vomiting, wheezing, changing color, cannot catch a breath, change in respiratory rate, change in oxygen needs, decrease in pulse oximeter readings, increased restlessness, unexplained irritability, discomfort, or abdominal pain, cannot talk, or you see the tube coming out of the mouth: Do not start the feeding.
- Make sure that the mark on the tube is at the nostril. Measure the tube from the mark at the nostril to the beginning of the hub and make sure it matches the "extra tube length" number you wrote down earlier. (See "Get ready," step 7, above.) If you cannot see the mark or the length has changed, do not start the feeding.
- Check placement with a pH strip. Try to pull out some stomach fluids with the syringe. Using a small syringe (3 to 5 ml) will make this easier. Test the acidity of the stomach fluids with a pH strip. A pH between 1-5.5 indicates proper placement. A pH of 6 or higher may indicate incorrect placement. If you get a pH of 6 or higher, DO NOT START THE FEEDING. Call Children’s Home Care to have the tube replaced.
- If having trouble getting pH, place your child on their left side for 15 minutes to allow stomach fluids to pool at the end of the tube.
- Write down pH level.
- Gently flush the tube with the amount of water prescribed by your provider.
- If unable to obtain pH but length, measurement and child's condition are unchanged, you may start the feeding.
Paying careful attention to these signs will help you to be sure the tube is placed correctly. If you have any doubts, it is best to remove the tube and replace it.
Safety Precautions
- Be aware the feeding set tubing can get wrapped around a child's neck, which could lead to strangulation or death.
- When running a feeding for your child, place the tubing in a way the tubing cannot get tangled around your infant or child. Place the tubing through your child's clothing or towards the foot of the bed. This will help the tubing from getting wrapped around your child's neck if they are to turn or move.
- If your child is injured by feeding set tubing, report the event to the FDA at [email protected] or call 1-800-638-2041.
Giving the feedings
___ Bolus feeding
It may be helpful to have 2 people to do this type of tube feeding. One person can hold and comfort the child while the other gives the feeding.
- Wash your hands.
- Measure the correct amount of formula and warm it to the desired temperature. Do not use the microwave to warm the feeding.
- Check tube placement as above (observing mark on NG tube and pH testing).
- Pinch the tube.
- Attach a syringe to the feeding tube.
- Pour the formula into the syringe.
- Unpinch the tube.
- Allow the formula to run for the same amount of time as it would take the child to drink it by mouth, or as prescribed by the doctor.
- Ways to help the feeding flow:
Try to start the feeding when the child is calm. You may have to "push" the feeding to get it started. To do this, place a plunger into the syringe and push slightly. Remove the plunger gently and allow the formula to flow in by gravity. If your child is crying, you may need to repeat the push several times.
___ A pacifier may help calm a young child and also helps to connect sucking with stomach-filling.
___ For older children, use activities to distract them, or involve the child with the feeding, such as holding the syringe. - During the feeding, keep the bottom of the syringe no higher than 6 inches above the child's stomach. The height of the syringe controls the feeding rate or speed.
- Continue adding formula into the syringe until the prescribed amount is given.
- When the syringe is empty, flush the tube with the prescribed amount of warm water.
- After the feeding:
___ Close the cap on the tube.
___ Leave the tube open to air. Tape a piece of gauze over the syringe to keep fluids from splashing out.
___ Burp your child.
___ Infants and young children may be most comfortable with their head and upper body raised, or lying on their left side.
___ Older children may be up and playing.
___ Continuous feeding with a feeding pump
- Wash your hands.
- Measure enough formula for 4 hours and warm it if needed. Do not use the microwave to warm feeding.
- Pour formula into the feeding bag. Run formula to the end of the pump tubing.
- Set up the pump and pump tubing according to the directions from the medical supply company. Be sure the rate is set correctly.
- If a new feeding tube is to be inserted, see "Getting ready to insert the tube" and "Inserting the tube."
- Check placement if external tube length measurement is unchanged, exit site mark is visible and there are no changes in your child's condition, continue feedings without interruption (see "Checking the tube placement"). If vomiting or respiratory distress occurs at any time, tube placement should be verified.
- Connect the pump tubing to the child's feeding tube.
- Turn on the pump. Check to make sure the formula is dripping.
- As the bag empties every 4 hours, add more formula.
- Hold and/or talk to your child often during waking hours. Have your child's head raised during the entire feeding.
- Watch your child carefully to make sure there is no change in breathing or behavior. Make sure the mark on the tube is still at the nostril. It is also a good idea to measure it every few hours, because sometimes the tube can slip under the tape. Stop the feeding if the mark changes and recheck placement.
- If your doctor tells you to, after the feeding period, flush the tube with the prescribed amount of warm water.
- If you are told to stop the continuous feeding:
___ Plug or clamp the tube.
___ Leave the tube open to air. Tape a piece of gauze over the syringe to keep fluids from splashing out.
___ Burp your child.
___ Have child's head raised for about 30 minutes after the feeding is done.
___ Removing the feeding tube (if ordered)
- Remove the tape.
- Pinch the tubing and pull the tube out in one quick motion.
- Hold, cuddle, and comfort your child. If your child is an infant, burp him or her.
Skin care
Clean your child's skin around the tube often with warm water, removing any secretions. If the nostril is reddened or the skin is irritated, remove the tube and replace it in the other nostril, if possible.
If you have used a transparent dressing on your child's face, remove it by loosening it with mineral oil and gently working the dressing off. If you use adhesive remover to loosen the dressing, be sure to wash the skin with water to remove all residue, as this can be very irritating.
Problem solving
| Problem | What to do |
| Clogged or plugged feeding tube (follow only the checked instructions) |
|
| Feeding tube falls out |
|
|
Coughing while tube is in place |
|
| Diarrhea and cramping |
|
| Nausea (upset stomach) or vomiting (throwing up) |
|
| Skin around the nose is irritated |
|
| Cannot obtain pH reading |
|
When should I call the doctor?
- fever
- vomiting or diarrhea that does not stop
- fussiness, hard to console
- pain or unusual distension in abdomen
- questions about using the tube
- trouble breathing - call 911
If you are concerned about your child for any reason, call your doctor to discuss the symptoms.
Questions?
This is not specific to your child, but provides general information. If you have any questions, please call your doctor, home care nurse, or dietitian.
Children's Minnesota
Reviewed 10/2022
This page is not specific to your child, but provides general information on the topic above. If you have any questions, please call your clinic. For more reading material about this and other health topics, please call or visit Children's Minnesota Family Resource Center library, or visit www.childrensmn.org/educationmaterials.
© 2024 Children's Minnesota
