The diagnosis and management of these lesions can be challenging in the prenatal period. Some of these babies may require urgent fetal intervention, so a thorough understanding of the possible treatment strategies is crucial for successful management of these patients.
Who will be on my care team?
At Midwest Fetal Care Center, a collaboration between Children’s Minnesota and Allina Health, we specialize in individual attention that starts with you having your own personal care coordinator to help you navigate this complex process. We use a comprehensive team approach to congenital lung malformations. That way, you are assured of getting the best possible information by some of the most experienced physicians in the country. For CLM, your care team will include a maternal-fetal specialist, a pediatric surgeon, a neonatologist, a nurse specialist care coordinator, a fetal care clinical social worker, and several other technical specialists. This entire team will follow you and your baby closely through the evaluation process and this team will be responsible for designing and carrying out your complete care plan.
Meet the team
What causes CLM?
Like most birth defects, it’s unknown what causes congenital lung malformations. There are rare familial cases where a parent or a relative may be affected, but in most cases, we don’t know the cause of CLM.
How is CLM diagnosed?
Congenital lung malformations are diagnosed by ultrasound (US). CLM can be detected by ultrasound as early as 16 weeks in pregnancy. When an abnormal mass is seen within the lungs of the developing fetus, CLM is confirmed.
How is CLM managed before birth?
The growth of congenital lung malformations can be variable and unpredictable. That is why our prenatal management of babies with CLM centers on monitoring your baby frequently by using several different techniques such as high resolution ultrasound, fetal echocardiography and MRI. This testing allows us to gather as much information about your baby as possible.
Although the prenatal behavior of CLM’s can be variable, two general patterns are seen. Nearly two thirds of these lesions experience a pattern of growth from 18 to 26 weeks gestation followed by a growth stoppage, often with shrinking after 30 weeks. The other one third remains stable in size and tend to shrink later in the pregnancy. A small number of fetuses with CLM may experience rapid growth during 18-26 weeks; these are the potentially symptomatic lesions which need even closer monitoring and may require a fetal intervention.
What is high resolution fetal ultrasonography?
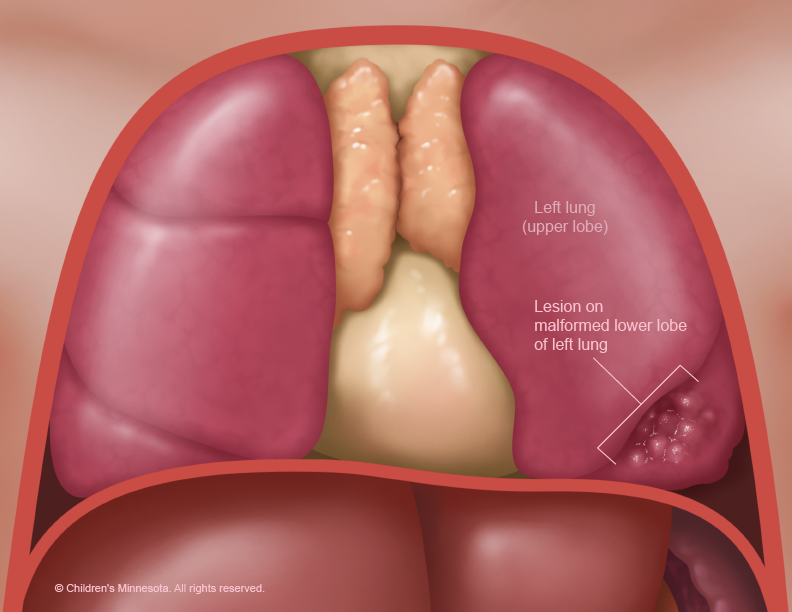
High resolution fetal ultrasonography (US) is a non-invasive test performed by one of our ultrasound specialists. The test involves looking at your baby through the mother’s abdomen using an ultrasound probe. If we see an abnormal mass within the lungs of the developing fetus, CLM is confirmed. It is important to classify the cysts as macrocystic (> 5mm in diameter for single or multiple cysts) or microcystic. This is because there are differing treatment options and outcomes for the different types of lesions.
What is the CAM Volume Ratio (CVR) and how is it used for babies with CLM?
The CVR is an important measurement that helps us to predict how severe your baby’s CLM may be. It is obtained by measuring the total mass of the baby’s lung lesion and dividing by the head circumference. Although there is no national consensus on a CVR value which is predictive of symptoms, the CVR is a useful tool to help us manage your baby’s CLM.
Generally, low CVR (less than 1.0) is associated with less severe disease, while a CVR > 1.6 causes us to consider possible interventions while your baby is still inside.
What is a fetal echocardiogram?
Fetal echocardiography (“echo” for short) is performed at our center by a pediatric cardiologist (physician who specializes in fetal heart abnormalities). This is a non invasive high resolution fetal ultrasound that involves looking specifically at your baby’s heart through the mother’s abdomen using an ultrasound probe. This test is important because seeing changes in blood flow through the heart also helps us to decide which babies may need treatment for CLM.
What is a fetal MRI?
MRI stands for magnetic resonance imaging. It is another non-invasive test we use to find out as much information as possible about your baby’s CLM. This test involves the mom and baby being scanned while partially inside our MRI machine. The test is a bit loud, but only takes a few minutes and is not uncomfortable.
What happens after my evaluation is complete?
After we have gathered all the anatomic and diagnostic information, our full team will meet to discuss the results of all your testing and then share our recommendations with you. Our approach for fetuses with CLM is twofold. First, we monitor the mother and the baby very closely during pregnancy looking for any significant growth of the lesion or potential complications of the lesion. Secondly, we use CVR to predict the severity of CLM based on ultrasound findings. This way, we are always prepared to optimally care for your unborn baby.
How can CLM be treated before birth?
Over 95% of babies with CLM will not require any special treatment during pregnancy or immediately after birth. These children will have no symptoms whatsoever and are treated with “expectant management” which means we are not recommending any procedures or interventions during the pregnancy. Instead, we are recommending continued close ultrasound surveillance to look for any changes that might cause us to change our plan.
A small number of babies with large CLM will require some type of therapy during pregnancy.
- What is betamethasone?
Betamethasone is a steroid and is the initial intervention that we consider in patients with large, solid or microcystic CLMs. This therapy yields a variable but generally positive response in either slowing the growth of the lesion or in causing it to shrink. The administration of steroids is a two dose regimen of betamethasone given to mom 24 hours apart. The exact mechanism as to how betamethasone affects the CLM is not clearly defined.
- What is cyst drainage?
For large, symptomatic macrocystic lesions, we would consider a minimally invasive approach to drain the large lesions. This can be accomplished via ultrasound guided cyst aspiration or placement of a tube into the lesion to drain it into the baby’s gestation sac (a thoracoamniotic shunt). Cyst aspiration quickly removes fluid inside of the CLM, however it is frequently only temporary and reaccumulation of the fluid within 48-72 hours is common. The use of a thoracoamniotic shunt may be a better option as it allows for continuous drainage. Practically, shunt movement after placement is common (usually caused by the baby) and may necessitate a repeat procedure.
- What is open fetal surgery for CLM?
Open fetal surgery has been used for removal of very high risk lung lesions. This is extremely rare would only be considered if we thought your baby may die without an intervention. These procedures are considered on a case by case basis and are usually offered prior to 30 weeks gestation.
How is CLM treated after birth?
Our goal for every patient is to have your baby get as close to your due date as possible. Most babies with CLM are born vaginally near term. If we have decided that your baby is at very low risk for any symptoms after birth, we will recommend that you can deliver at any hospital close to your home that offers at least Level 2 NICU service.
If your baby has a bigger CLM, we will recommend that your baby will be born at one of our specialized mother-baby centers. Children’s Minnesota is one of only a few centers nationwide with the birth center located within the hospital complex. This means that your baby will be born just a few feet down the hall from our newborn intensive care unit (NICU). If necessary, many of the physicians you have already met may be present during or immediately after your baby’s birth so we can care for your baby right away.
When will my baby have the CLM operation?
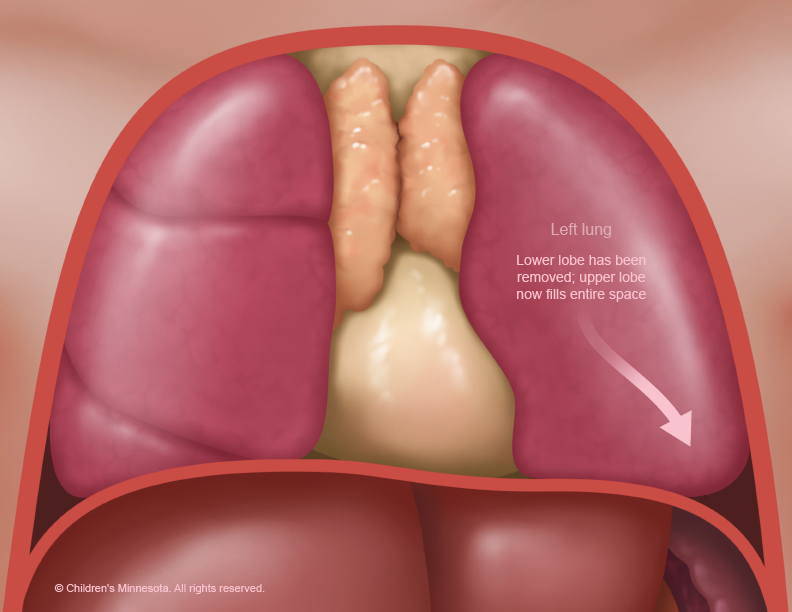
The abnormal lung tissue will need to be surgically removed. However, this surgery is almost never an emergency and frequently it is delayed for a few months until we are certain that your baby is feeding and growing normally and is in the best possible condition for surgery.