Who will be on my care team?
At Midwest Fetal Care Center, a collaboration between Children’s Minnesota and Allina Health, we specialize in individual attention that starts with you having your own personal care coordinator to help you navigate your baby’s complex treatment process. We use a comprehensive team approach to tracheoesophageal fistula and esophageal atresia (TEF/EA). That way, you are assured of getting the best possible information by some of the most experienced physicians in the country. For TEF/EA, your care team will include a maternal-fetal specialist, a pediatric surgeon, a neonatologist, a geneticist, a nurse specialist care coordinator and several other technical specialists. This entire team will follow you and your baby closely through the evaluation process, and will be responsible for designing and carrying out your complete care plan.
Meet the team
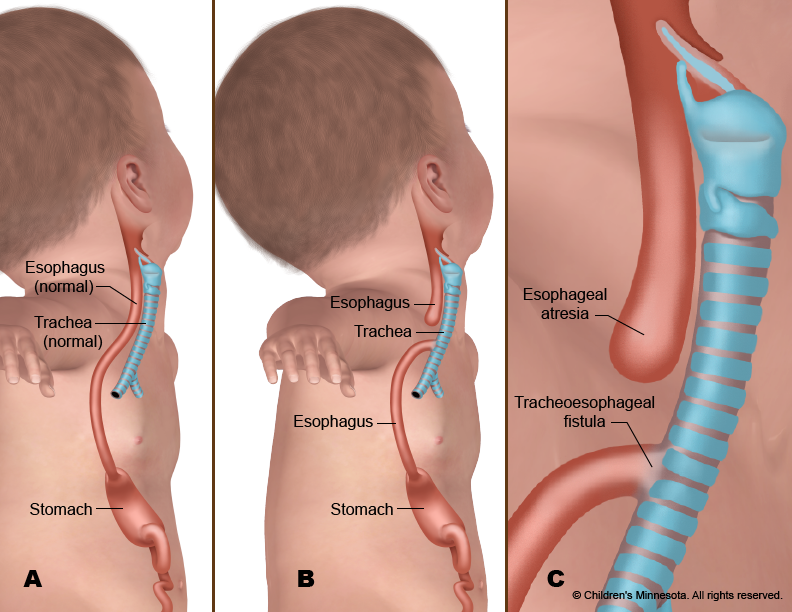
What causes tracheoesophageal fistula/esophageal atresia?
TEF/EA is a congenital condition, which means it develops before birth. Exactly what causes it is unknown, although genetics may play a role in rare cases.
How is tracheoesophageal fistula/esophageal atresia diagnosed?
Tracheoesophageal fistula and esophageal atresia diagnosis can sometimes be made by ultrasound during pregnancy. The ultrasound might show that the baby has an abnormally small stomach. Or it might show that there is an excessive amount of amniotic fluid in the womb. Both are potential tracheoesophageal fistula/esophageal atresia symptoms. If these signs are present, a more detailed ultrasound may be done to see if the condition can be confirmed. Usually, however, a diagnosis cannot be made with certainty until after the baby is born.
How is tracheoesophageal fistula/esophageal atresia managed before birth?
The prenatal management of babies with TEF/EA starts with acquiring as much information about the condition—and possible co-existing VACTERL conditions—as early as possible. To gather that information, we use several different techniques, including high-resolution fetal ultrasonography, fetal echocardiography and fetal magnetic resonance imaging (MRI).
What is high-resolution fetal ultrasonography?
High-resolution fetal ultrasonography is a non-invasive test performed by one of our ultrasound specialists. The test uses reflected sound waves to create images of the baby within the womb. We will use ultrasonography to follow the development of your baby’s internal organs throughout your pregnancy so that an accurate diagnosis of tracheoesophageal fistula and esophageal atresia can be made as soon as possible. It will also help us identify other VACTERL birth defects that might be present.
What is fetal echocardiogram?
Fetal echocardiography (“echo” for short) is performed at our center by a pediatric cardiologist (a physician who specializes in fetal heart abnormalities). This non- invasive, high-resolution ultrasound procedure looks specifically at how the baby’s heart is structured and functioning while in the womb. This test is important because babies with TEF/EA sometimes have a heart-related birth defect as well.
What is fetal MRI?
Fetal MRI is another non-invasive test. It uses a large magnet, pulses of radio waves and a computer to create detailed images of your baby’s organs and other structures while in the womb. This procedure involves both mom and baby being scanned while partially inside our MRI machine. The test is a bit loud, but it takes only a few minutes and is not uncomfortable.
What happens after my evaluation is complete?
After we have gathered all the anatomic and diagnostic information from the tests, our full team will meet with you to discuss the results. Tracheoesophageal fistula and esophageal atresia treatment cannot begin until after the child is born. We will, however, take an active, twofold approach to managing the condition during your pregnancy. First, we will monitor both mother and baby very carefully during pregnancy, looking for any potential complications that might lead to premature delivery. Second, we will try to predict the severity of tracheoesophageal fistula and esophageal atresia based on the ultrasound and MRI findings so we can be prepared during and after delivery to optimally care for your infant.
How is tracheoesophageal fistula/esophageal atresia treated after birth?
Infants with tracheoesophageal fistula and esophageal atresia can be delivered vaginally. Our goal will be to have your baby’s birth occur as near to your due date as possible. Your baby will be born at The Mother Baby Center at Children’s Minnesota and Abbott Northwestern. Children’s Minnesota is one of only a few centers nationwide with a birth center located within the hospital complex. This means that your baby will be born just a few feet down the hall from our newborn intensive care unit (NICU). Also, many of the physicians you have already met will be present during or immediately after your baby’s birth to help care for your baby right away.
Most babies with TEF/EA are comfortable breathing on their own after birth. But your baby will be unable to nurse or take a bottle and will be fed intravenously instead. In addition, a small suction tube will be inserted into your baby’s esophageal “pouch” to keep the saliva your baby swallows from entering the trachea and overflowing into the lungs.
Our goal will be to make a definitive diagnosis of TEF/EA as quickly as possible. The diagnosis can be made with a simple x-ray, done soon after birth. Other tests, including an ultrasound scan and an echocardiogram, will also be conducted to identify any co-existing VACTERL conditions.
When will my baby have an operation?
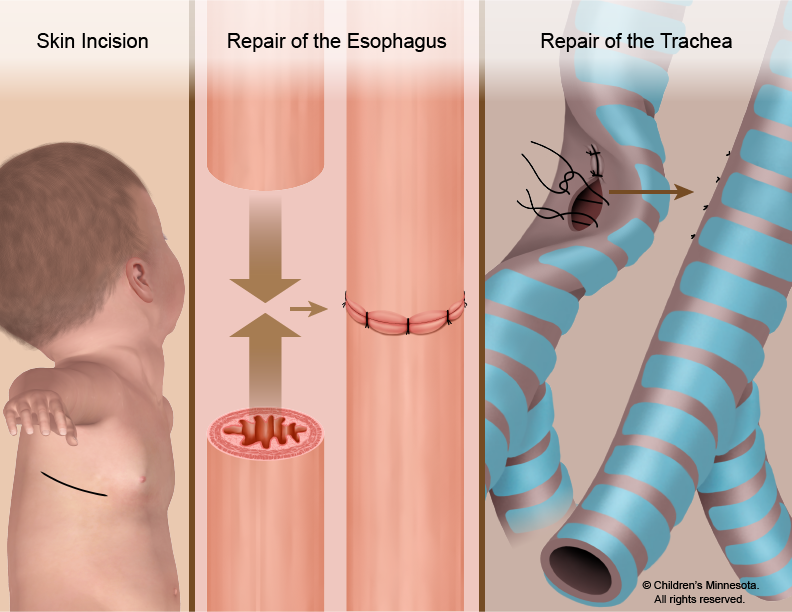
Tracheoesophageal fistula and esophageal atresia repair requires an operation to close the fistula and repair the esophagus and trachea. Surgery for esophageal atresia is not considered an emergency, and is typically done when the baby is two or three days old.
In most cases of tracheoesophageal fistula and esophageal atresia repair, the surgeon cuts through the abnormal connection (fistula) between the windpipe and esophagus and then sews together the two ends of the esophagus. The windpipe is also repaired. But the exact nature of your baby’s surgery will depend on the specific defects in your baby’s digestive tract.
The surgery is done under general anesthesia. After the procedure, your baby will be returned in the NICU. For several days, your baby may need a machine (ventilator) to help with breathing.