Who will be on my care team?
At Midwest Fetal Care Center, a collaboration between Children’s Minnesota and Allina Health, we specialize in individual attention that starts with you having your own personal care coordinator to help you navigate your baby’s complex treatment process. We use a comprehensive team approach to gastroschisis. That way, you are assured of getting the best possible information by some of the most experienced physicians in the country. For gastroschisis treatment, your care team will include a maternal-fetal specialist, a pediatric surgeon, a neonatologist, a geneticist, a nurse specialist care coordinator, a fetal care clinical social worker, and several other technical specialists. This entire team will follow you and your baby closely through the evaluation process, and will be responsible for designing and carrying out your complete gastroschisis treatment plan.
Meet the team
What causes gastroschisis?
Like most birth defects, it’s unknown what causes gastroschisis. There are rare familial cases where a parent or a relative may be affected, but in most cases, we don’t know the cause of gastroschisis.
How is gastroschisis diagnosed?
Gastroschisis is diagnosed by ultrasound (US). This US may have been requested by your primary doctor because you had an increased level of alpha fetal protein (AFP) in your blood. Alternatively, gastroschisis may be diagnosed by a routine US after approximately 10-12 weeks of pregnancy. When abdominal organs such as the intestines or stomach are seen floating freely outside of the abdominal cavity of the developing fetus, gastroschisis is confirmed. Unfortunately, we still see a few patients each year who are not diagnosed until birth. When this occurs, the newborn must be immediately transported to a center capable of managing gastroschisis emergency treatment.
How is gastroschisis managed before birth?
Although there is no specific prenatal treatment for babies with gastroschisis, we have a comprehensive approach to managing these pregnancies starting with diagnosis. Our prenatal management centers on acquiring as much information about your baby as possible. We accomplish that by using high resolution fetal ultrasound.
What is high-resolution fetal ultrasonography?
High-resolution fetal ultrasonography is a non-invasive test performed by one of our ultrasound specialists. The test uses reflected sound waves to create images of the baby within the womb. When abdominal organs such as the intestines or stomach are seen floating freely outside of the abdominal cavity of the developing fetus, gastroschisis is confirmed. A finding of intra-abdominal bowel dilatation sometimes suggests complicated gastroschisis, where a portion of the bowel may be blocked (called an atresia). In addition to the intestinal measurements, we will also check many other measurements that will help us to tell how your baby is being affected by the gastroschisis.
What happens after my evaluation is complete?
After we have gathered all the anatomic and diagnostic information about your baby, our full team will meet to discuss the results of all your testing and then share our recommendations and options for gastroschisis treatment with you. Our approach for fetuses with gastroschisis is twofold. Firstly, we monitor the mother and the baby very carefully during pregnancy looking for any potential complications, such as premature labor or excessive amounts of amniotic fluid that might lead to premature delivery. Babies with gastroschisis are also more likely to be growth restricted so we will follow the growth carefully. Secondly, we try to predict the severity of gastroschisis based on ultrasound findings so we can be prepared during and after delivery to optimally care for your infant.
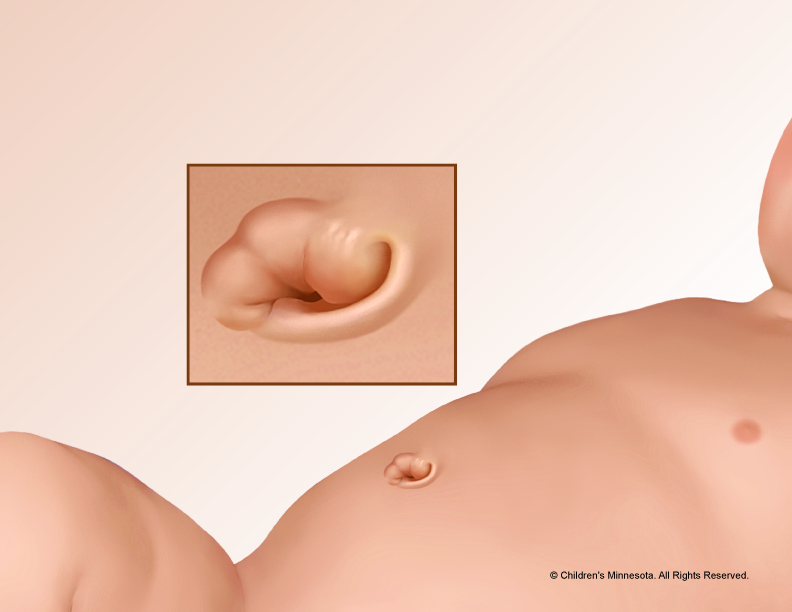
How is gastroschisis treated after birth?
The average pregnancy with gastroschisis delivers between 35 and 38 weeks. If your baby has not delivered by 38 weeks, we will “induce” the pregnancy to cause delivery because there is some evidence that the last few weeks of pregnancy may be more dangerous for babies with gastroschisis. Most babies with gastroschisis are born naturally through the birth canal. Your baby will be born at The Mother Baby Center at Children’s Minnesota and Abbott Northwestern. Children’s Minnesota is one of only a few centers nationwide with a birth center located within the hospital complex. This means that your baby will be born just a few feet down the hall from our newborn intensive care unit (NICU). Also, many of the physicians you have already met will be present during or immediately after your baby’s birth to help care for your baby right away.
Most often, babies with gastroschisis do not have any problems with their hearts or lungs, so they are comfortable breathing on their own after birth. Immediately after birth, our goal is to get your baby wrapped and transported to our newborn intensive care unit as quickly as possible.
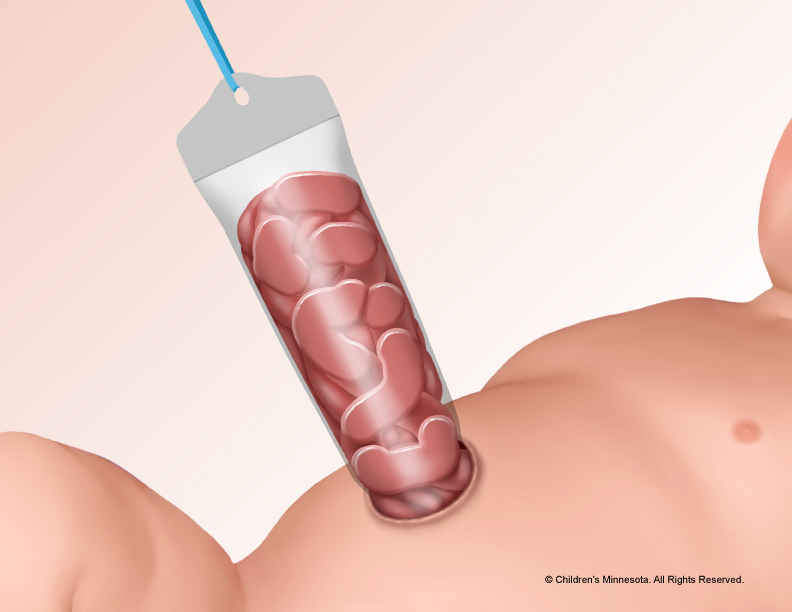
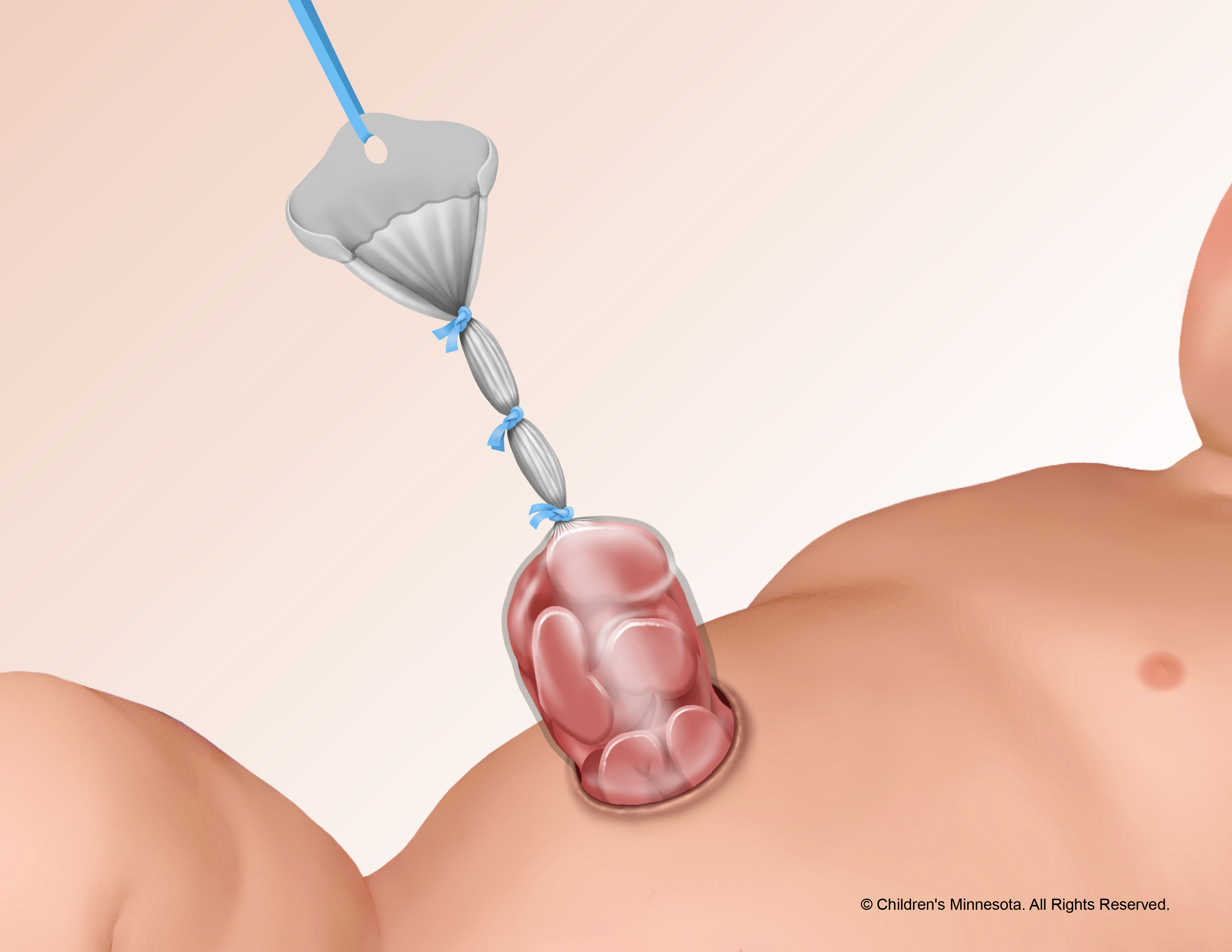
What is a silo?
A silo is a specially made piece of plastic that can be placed over the bowels to protect them before surgery, as part of gastroschisis treatment. Most babies with gastroschisis will need a temporary silo to house the intestines. Sometimes it is just for a few hours until your baby is ready for surgery and other times the silo may in place for several days while we wait for the intestines to shrink enough to fit back into the abdomen. The silo can usually be easily placed at your baby’s bedside.