How is lower urinary tract obstruction (LUTO) diagnosed?
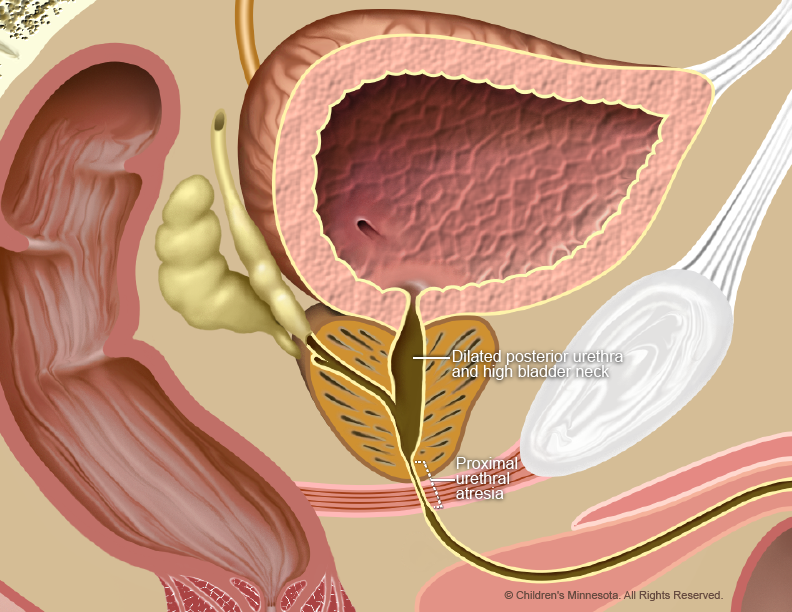
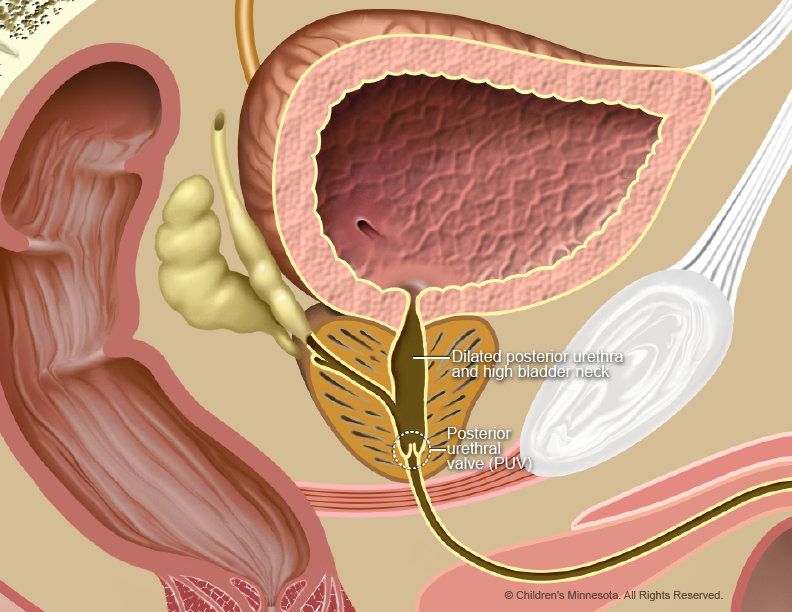
LUTO is diagnosed during routine prenatal ultrasounds. The baby’s bladder may look larger than normal on the ultrasound, and its muscular walls may appear extra thick due to the pressure of the urine. In cases involving PUVs, the bladder may have a “key-hole” shape.
The ultrasound may also show higher-than-normal amounts of fluid in the baby’s kidneys. In severe cases, the kidneys and bladder may have ruptured, and fluid may have filled the baby’s abdomen. LUTO may also be suspected if abnormally low levels of amniotic fluid (oligohydramnios) appear on the ultrasound image.
How is lower urinary tract obstruction (LUTO) managed before birth?
The prenatal management of babies with LUTO starts with acquiring as much information about the condition as early as possible. To gather that information, we may recommend one or more prenatal screening techniques, including high-resolution fetal ultrasonography, fetal magnetic resonance imaging (MRI), fetal echocardiography, amniocentesis, and possible assessment of the baby’s kidney function through a renal function panel.
What is high-resolution fetal ultrasonography?
High-resolution fetal ultrasonography is a non-invasive test performed by one of our ultrasound specialists. The test uses reflected sound waves to create images of the baby within the womb. We will use ultrasonography to follow the development of your baby’s urinary tract and other internal organs and the volume of amniotic fluid that surrounds your baby throughout the pregnancy.
What is fetal magnetic resonance imaging (MRI)?
Fetal MRI is another non-invasive test. It uses a large magnet, pulses of radio waves and a computer to create detailed images of your baby’s urinary tract and other structures while in the womb. This procedure involves both mom and baby being scanned while partially inside our MRI machine. The test is a bit loud, but it takes about 30 minutes and is not uncomfortable.
What is fetal echocardiography?
Fetal echocardiography (“echo” for short) is performed at our center by a pediatric cardiologist (a physician who specializes in fetal heart abnormalities). This non-invasive, high-resolution ultrasound procedure looks specifically at how the baby’s heart is structured and functioning while in the womb. This test is important because babies with birth defects are at increased risk of heart abnormalities. A fetal echocardiogram is also a necessary part of the evaluation process when prenatal surgery is being considered.
What is amniocentesis?
If your baby is found to have LUTO, your doctor will offer you an amniocentesis test to see if your baby has any associated genetic or chromosomal condition that would exclude him or her from being a candidate for prenatal surgery. This test is a necessary part of the evaluation process when prenatal surgery is being considered. For this procedure, a small sample of fluid will be removed from the amniotic sac surrounding your baby. The amniotic fluid will contain cells from your baby, and in those cells will be your baby’s chromosomes for us to analyze. The procedure is straightforward and can be done in our clinic. It requires placing a small needle through the abdomen and into the amniotic sac to obtain the fluid sample. Test results will take several days for our laboratory to process.
What is a renal function panel?
This test helps determine how the baby’s kidneys are functioning and whether the baby is a candidate for potential intervention. The procedure, which can be done in our clinic, involves inserting a small needle through the mother’s abdomen and into the baby’s bladder. The bladder is then drained of urine (a process known as vesicocentesis), and a sample of the urine is tested for its electrolyte levels. Electrolytes — such nutrients as potassium, phosphate, magnesium, calcium, and sodium — are essential for the healthy functioning of kidneys. For accurate results, the procedure may need to be repeated at one- to two-day intervals.
What happens after my evaluation is complete?
After we have gathered all the anatomic and diagnostic information from the tests, our full team will meet with you to discuss the results and whether treatment is feasible. The treatment option that will be best for your baby will depend on several factors, including the cause, location, and severity of the urinary tract blockage. Your child’s medical team will design a treatment plan tailored to your child’s specific needs.
How is lower urinary tract obstruction (LUTO) treated before birth?
One of the prenatal treatments for LUTO is expectant management. This involves continued close ultrasound surveillance throughout the pregnancy, but no surgical intervention. We currently recommend expectant management if the amniotic fluid levels remain normal.
The goal of surgical prenatal treatments for LUTO is to prevent urine buildup and keep amniotic fluid levels at normal levels, thus reducing the risk of damage to the baby’s lungs. These treatments include the following:
- A needle is used to drain excess urine from the baby’s bladder. The procedure may need to be repeated several times during the pregnancy.
- Vesicoamniotic shunting. A small, hollow needle is inserted through the mother’s abdomen and into the baby’s bladder. A tiny shunt is then sent through the tube and positioned at the lower end of the bladder. The shunt allows urine to flow from the bladder into the amniotic cavity. After the baby’s birth, when the urinary tract obstruction can be treated with other surgical options, the shunt is removed.
- Amnioinfusion. This procedure involves the injection of fluid into the amniotic cavity to restore normal fluid levels and improve lung development
- Fetoscopic laser surgery. A small incision is made in the mother’s abdomen, and a narrow tube-like instrument known as an endoscopeis inserted through the uterus and into the amniotic cavity. The endoscope has a tiny camera attached to it, which enables the surgeon to locate the blockage in the urinary tract. Laser energy is then sent down the endoscope, which the surgeon uses to cut away any tissue causing the blockage. This procedure is minimally available.
How is lower urinary tract obstruction (LUTO) treated after birth?
Our goal will be to have your baby’s birth occur as near to your due date as possible. Babies with LUTO can be delivered vaginally. If the baby has low levels of amniotic fluid, however, he or she is at increased risk during delivery of being in an abnormal position (not “presenting” head first) and of having temporary drops (decelerations) in their heart rate. Either of those situations may require a Cesarean section. During labor, your baby will be monitored closely, and your doctor will be prepared for all complications or outcomes.
Your baby may be born at The Mother Baby Center at Abbott Northwestern and Children’s Minnesota in Minneapolis or at The Mother Baby Center at United and Children’s Minnesota in St. Paul. Children’s Minnesota is one of only a few centers nationwide with a birth center located within the hospital complex. This means that your baby will be born just a few feet down the hall from our newborn intensive care unit (NICU). Also, many of the physicians you have already met will be present during or immediately after your baby’s birth to help care for your baby right away.
Your baby will need specialized medical care after birth and will therefore be taken to our NICU, where the baby’s condition will be assessed and respiratory and other support will be provided as needed. Our goal will be to make a definitive diagnosis of the location of the obstruction as quickly as possible. That diagnosis can be made with a simple x-ray and/or ultrasound imaging, done soon after birthWe will also determine the extent of damage to the baby’s kidneys, lungs, heart, and other organs.
After we have gathered all the information from the tests, our full team will meet with you to discuss your child’s results and postnatal treatment options. The type of treatment will depend on the type of obstruction.
- Babies born with severe lung and/or kidney damage will be offered palliative and hospice care.
- For babies with PUV and normal lung function, a minimally invasive surgical procedure known as PUV resection may be performed within the first few days after birth. A small incision is made in the baby’s abdomen, and an endoscope (a narrow tube-like instrument with a tiny camera) is inserted the urinary tract. Once the surgeon has located the flaps of tissue causing the blockage, laser heat is used to cut it away.
- Some babies many need urethral reconstruction surgery to reconstruct their urethra.
- A vesicostomy is sometimes done to drain the baby’s bladder of urine until the baby is healthy enough for PUV resection or urethral reconstruction surgery. For this procedure, a tube is inserted into the bladder through an opening below the baby’s belly button. The urine is drained into a diaper.
What is my baby’s prognosis?
The long-term prognosis for babies with LUTO depends on how much impact the condition had on the development of the baby’s kidneys and lungs. Babies born with LUTO are more susceptible to kidney infections and kidney failure. Many eventually require kidney transplants. They are also at a higher risk of bladder problems and of long-term respiratory illnesses, including upper respiratory infections and asthma. Babies that developed joint contractions due to low levels of amniotic fluid during gestation are susceptible to musculoskeletal problems.
Will my baby need long-term follow-up care?
Yes. Because of all the potential health issues associated with LUTO, your baby will require long-term follow-up care. We will work with you to develop a detailed care plan for your baby. The plan will be implemented by a comprehensive team of specialists, including a pediatrician (who will coordinate your baby’s overall care) and a pediatric kidney specialist.