What is Down syndrome (trisomy 21)?
Down syndrome is a genetic disorder. Babies born with the condition have an extra copy of chromosome 21, giving them three copies instead of the usual two. For that reason, Down syndrome is also known as trisomy 21. The extra chromosome alters the normal course of a child’s development, resulting in the physical features and mild to moderate intellectual disabilities associated with the condition. Children born with Down syndrome are more likely to have heart abnormalities and vision and hearing problems, as well as other health-related conditions. Due to medical and other advances, however, today’s children with Down syndrome can grow up to live long, happy, healthy and productive lives.
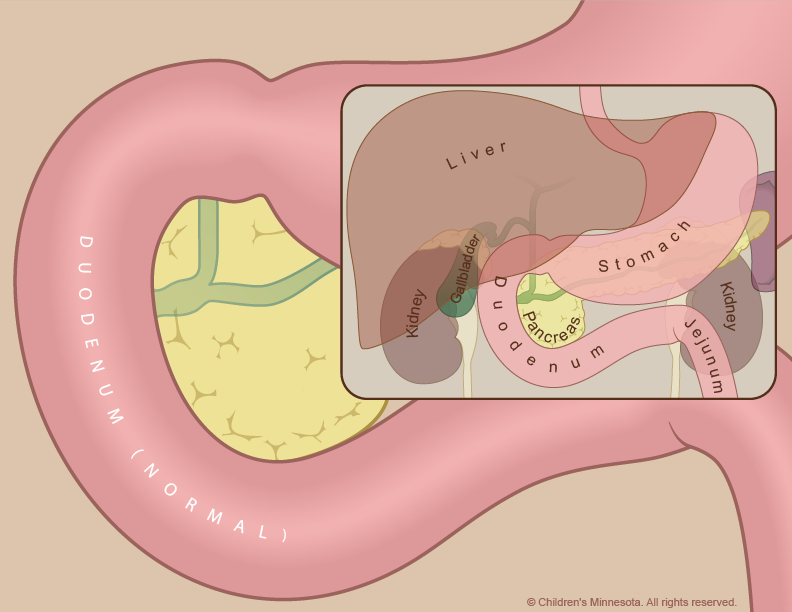
How is duodenal atresia managed before birth?
The prenatal management of babies with duodenal atresia starts with acquiring as much information about the condition as early as possible. Tests will also be done to help determine if Down syndrome or a heart-related birth defect are present. To gather all of that information, we use several different techniques, including high-resolution fetal ultrasonography, fetal echocardiography and amniocentesis.
What is high-resolution fetal ultrasonography?
High-resolution fetal ultrasonography is a non-invasive test performed by one of our ultrasound specialists. The test uses reflected sound waves to create images of the baby within the womb. We will use ultrasonography to follow the development of your baby’s intestinal tract — and other internal organs — throughout your pregnancy. We will also look for signs of excess amniotic fluid around your baby (known as polyhydramnios), which may raise the risk of an early delivery.
What is fetal echocardiogram?
Fetal echocardiography (“echo” for short) is performed at our center by a pediatric cardiologist (a physician who specializes in fetal heart abnormalities). This non- invasive, high-resolution ultrasound procedure looks specifically at how the baby’s heart is structured and functioning while in the womb. This test is important because babies with Down syndrome and duodenal atresia sometimes have a heart-related birth defect as well.
What is amniocentesis?
Amniocentesis is a test done during pregnancy to check if your baby has a genetic or chromosomal condition, such as Down syndrome. A small sample of fluid will be removed from the amniotic sac surrounding your baby. The amniotic fluid will contain cells from your baby, and in those cells will be your baby’s chromosomes for us to analyze. The procedure is straightforward and can be done in our clinic. It requires placing a small needle through the abdomen and into the amniotic sac to obtain the fluid sample. Test results will take several days for our laboratory to process. The information obtained from this test will be very important for creating your care plan and for helping the neonatologist care for your infant after birth.
What happens after my evaluation is complete?
After we have gathered all the anatomic and diagnostic information from the tests, our full team will meet with you to discuss the results. Duodenal atresia cannot be treated before a child is born. We will, however, take an active, two-fold approach to managing the condition during your pregnancy. First, we will monitor both mother and baby very carefully, looking for any potential complications that might lead to premature delivery. One of those potential complications is the accumulation in the uterus of extra amniotic fluid (polyhydramnios), which can occur when the atresia (blockage) makes it difficult for the baby to swallow. If this happens, we will watch closely for signs of preterm labor and/or symptoms in the mother related to the increased uterine size and pressure. Occasionally, an amnioreduction is performed. This procedure, which is similar to an amniocentesis, removes some of the excess fluid and alleviates any symptoms the mother may be experiencing.
Second, we will try to identify any complicating factors — such as Down syndrome or a heart defect — that might require additional therapies. That way we can be prepared during and after delivery to optimally care for your infant.
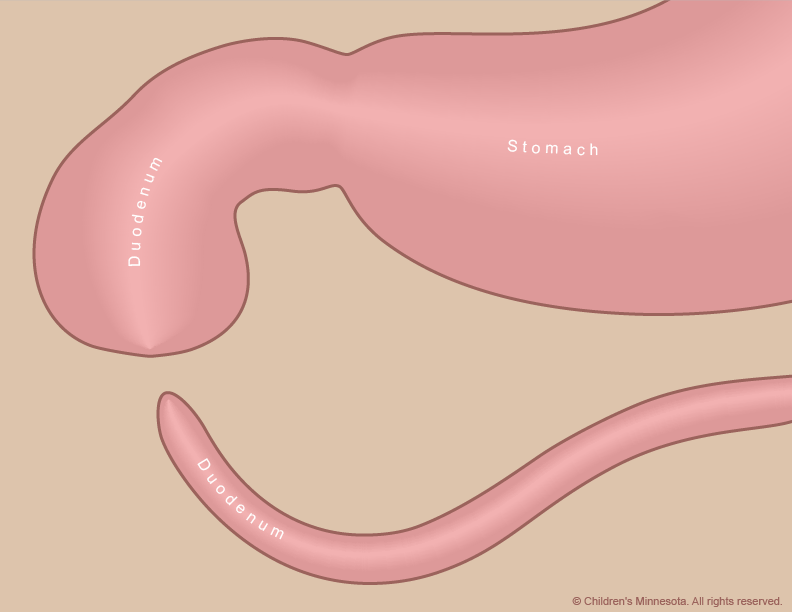
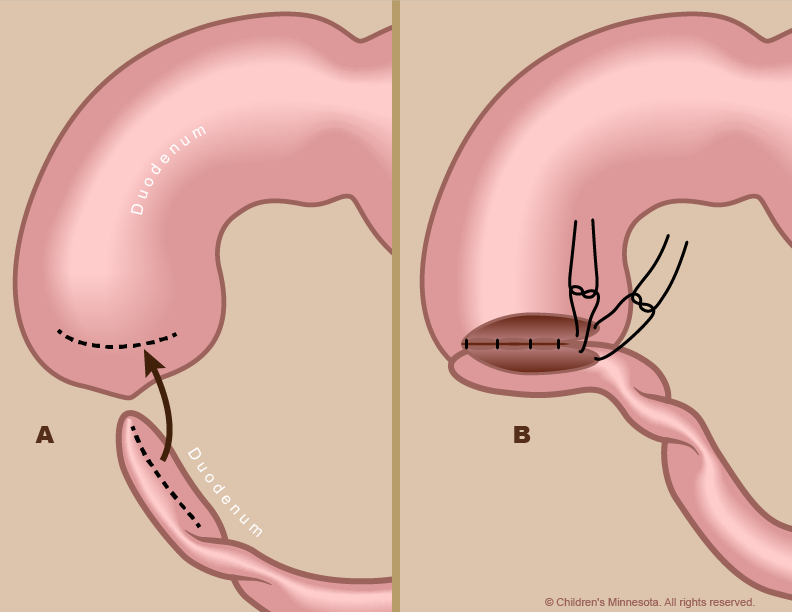
How is duodenal atresia treated after birth?
Infants with duodenal atresia can be delivered vaginally. Our goal will be to have your baby’s birth occur as near to your due date as possible. Your baby will be born at The Mother Baby Center at Abbott Northwestern and Children’s Minnesota in Minneapolis or at The Mother Baby Center at United and Children’s Minnesota in St. Paul. Children’s Minnesota is one of only a few centers nationwide with a birth center located within the hospital complex. This means that your baby will be born just a few feet down the hall from our newborn intensive care unit (NICU). Also, many of the physicians you have already met will be present during or immediately after your baby’s birth to help care for your baby right away.
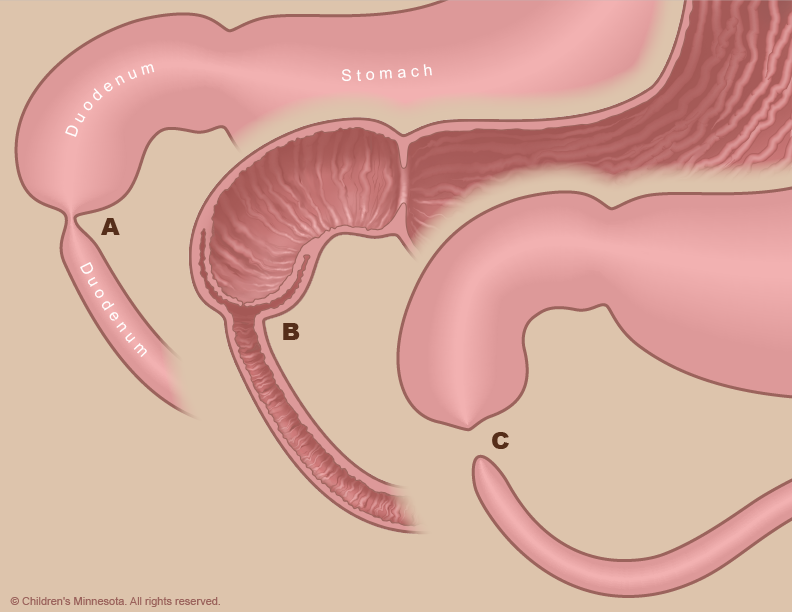
Your baby will need specialized medical care after birth and will therefore be taken to our NICU. Most babies with duodenal atresia are comfortable breathing on their own, but your baby will be unable to nurse or take a bottle and will be fed nutrients intravenously instead. Because your child’s intestine is blocked by the atresia, a thin flexible tube will be inserted into your baby’s stomach through either the nose or mouth. This tube will be used to suck out any air or fluid that collects in the child’s stomach.
Our goal will be to make a definitive diagnosis of duodenal atresia as quickly as possible. That diagnosis can be made with a simple x-ray, done soon after birth. An echocardiogram will also be conducted to identify any co-existing heart defect.