What causes a lymphatic malformation?
Lymphatic malformations are the result of problems that develop before birth in the vessels of the lymphatic system, which plays a central role in defending the body against infection and disease. The vessels drain watery fluid (lymph) from tissue and transport it to the lymph nodes, where bacteria, viruses and other harmful pathogens are destroyed. The vessels then send the cleaned-up fluid back into the bloodstream.
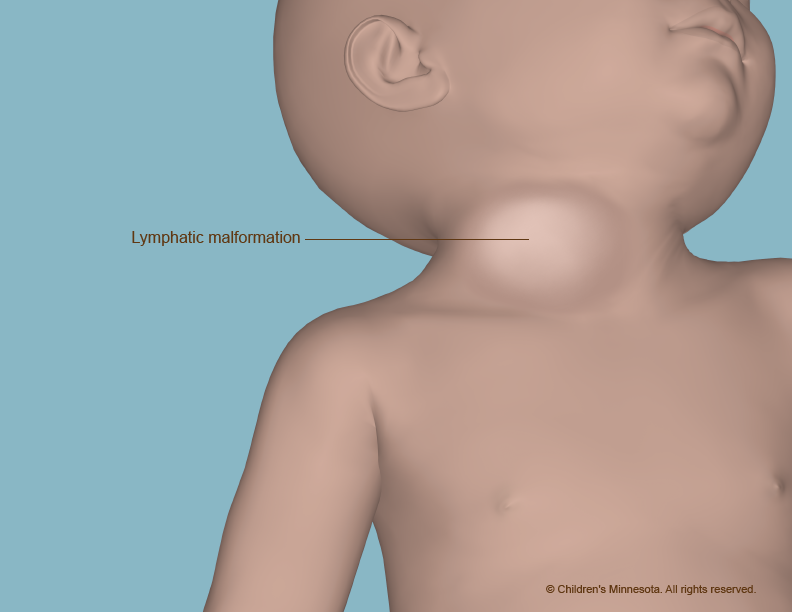
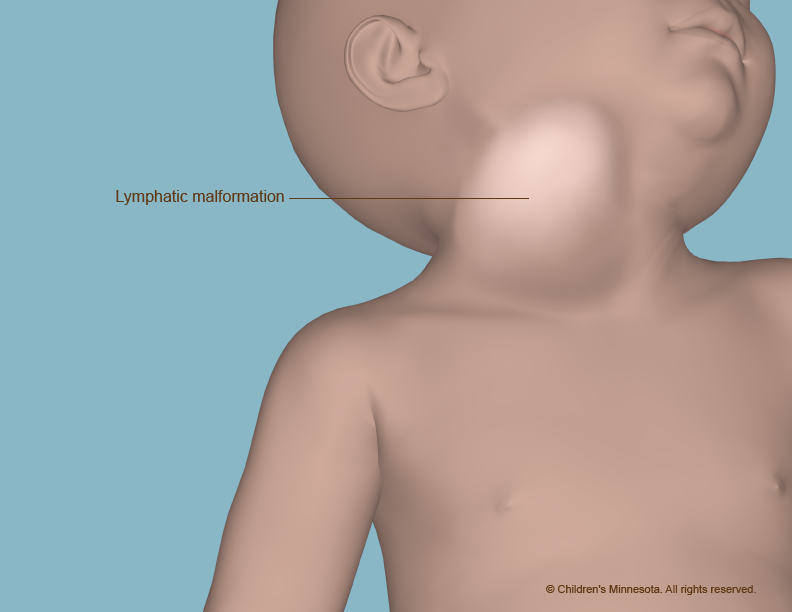
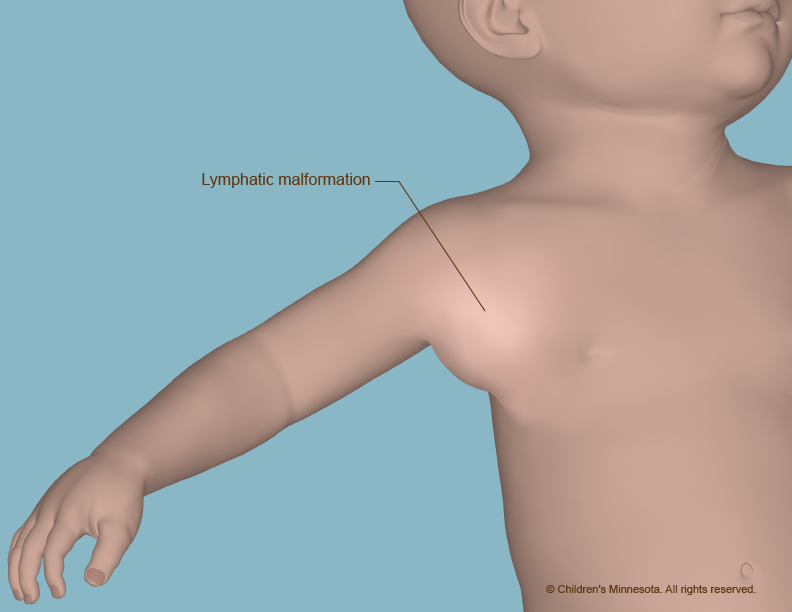
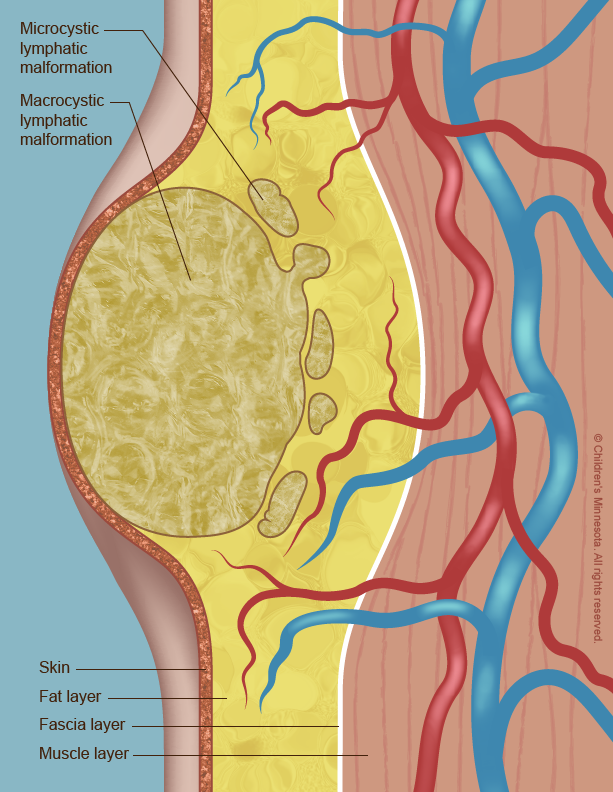
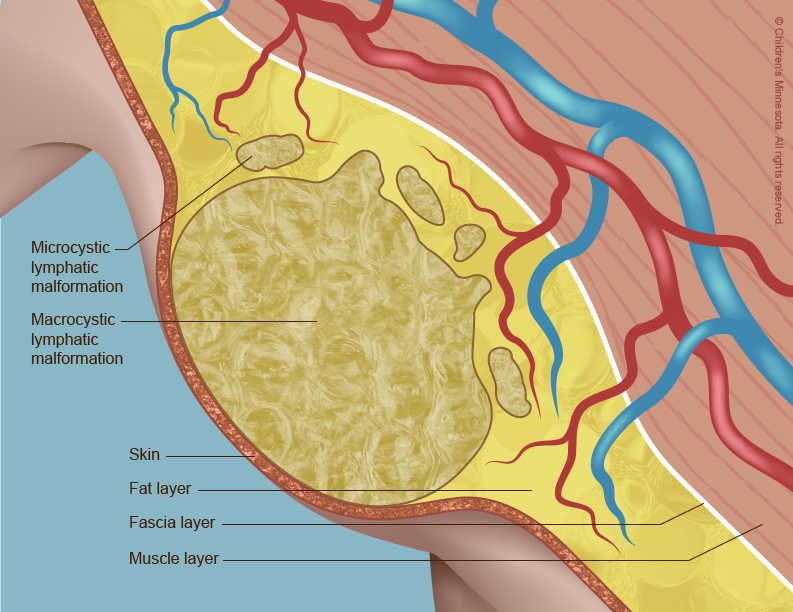
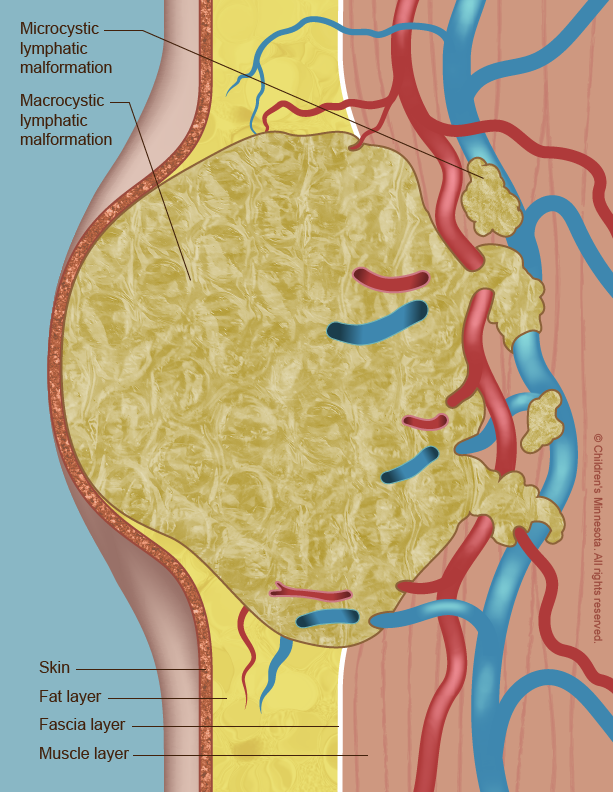
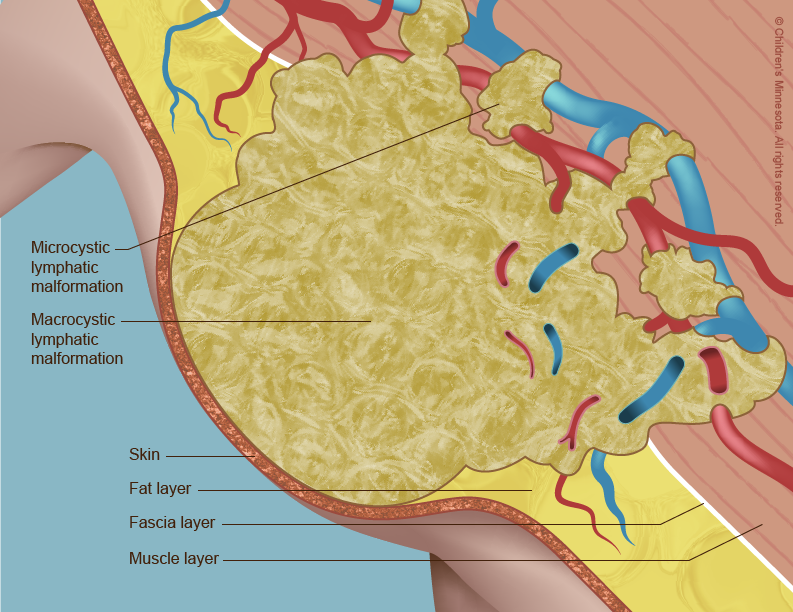
A lymphatic malformation occurs when the vessels do not form properly and become blocked and enlarged. Lymph then collects in them, leading to the creation of fluid-filled cysts. The cysts usually get bigger as the unborn baby grows, although sometimes they spontaneously shrink or even disappear.
When a lymphatic malformation is detected very early in pregnancy, it may be associated with a chromosomal anomaly, such as Down syndrome (trisomy 21), Turner syndrome or Noonan syndrome. It may also be associated with other birth defects, such as a heart defect. For these reasons, careful follow-up with ultrasound surveillance will be recommended.
How is a lymphatic malformation diagnosed?
Lymphatic malformations that present early in pregnancy typically form between the 9th and 16th week of pregnancy, and are often diagnosed during a routine prenatal ultrasound exam or genetic screening exam. You will be referred to a genetic specialist, as early lymphatic malformations may be associated with chromosomal abnormalities. A detailed ultrasound will also be recommended later in pregnancy to evaluate your baby’s anatomy, since an early lymphatic malformation may also indicate the presence of another birth defect. Part of that evaluation will be done by a pediatric cardiologist, who will assess the baby’s heart anatomy.
Lymphatic malformations that present later in pregnancy may be detected during a routine ultrasound, or your doctor may note that your abdomen appears larger than expected for your weeks in pregnancy and order an ultrasound. If your doctor suspects the presence of one of these malformations by ultrasound imaging, he or she may recommend further imaging tests, such as fetal magnetic resonance imaging (MRI), to evaluate the extent of the malformation and any possible impact it may be having on the development of the baby’s internal organs.
How is a lymphatic malformation managed before birth?
The prenatal management of babies with lymphatic malformations starts with acquiring information about the condition’s severity and possible association with a chromosomal anomaly. To gather this information, we may use several different technologies, including high-resolution fetal ultrasonography, fetal MRI, fetal echocardiography, amniocentesis and chorionic villus sampling (CVS). A genetic specialist will counsel you on the different options for detecting chromosomal abnormalities and a maternal-fetal specialist will discuss imaging and follow-up management.
What is high-resolution fetal ultrasonography?
High-resolution fetal ultrasonography is a non-invasive test performed by one of our ultrasound specialists. The test uses reflected sound waves to create images of the baby within the womb. We will use ultrasonography to follow the growth of your baby’s lymphatic malformation — and of any effect it may be having on your baby’s internal organs — throughout your pregnancy.
What is fetal magnetic resonance imaging (MRI)?
Fetal MRI is another non-invasive test. It uses a large magnet, pulses of radio waves and a computer to create detailed images of your baby’s organs and other structures while in the womb. This procedure involves both mom and baby being scanned while partially inside our MRI machine. The test is a bit loud, but it takes only about 30 minutes and is not uncomfortable.
What is fetal echocardiogram?
Fetal echocardiography (“echo” for short) is performed at our center by a pediatric cardiologist (a physician who specializes in fetal heart abnormalities). This non-invasive, high-resolution ultrasound procedure looks specifically at how the baby’s heart is structured and functioning while in the womb. This test is important because lymphatic malformations are sometimes associated with heart defects.
What is amniocentesis?
An amniocentesis is done to sample the amniotic fluid around your baby. This fluid will contain some of your baby’s cells, which will provide a full set of your baby’s chromosomes for us to analyze. We can then assess if the cause of the lymphatic malformation is related to a chromosomal anomaly. The amniocentesis procedure is straightforward and can be done in our clinic. It requires placing a small needle through the mother’s abdomen and into the amniotic sac to obtain the fluid sample. Getting final results from the test from our laboratory usually takes several days. The information will be very important for creating your care plan and helping the neonatologist care for your infant after birth.
What is chorionic villus sampling (CVS)?
This test involves taking a small sample of tissue from the placenta, which is attached to the uterus. Some of the placental cells are then tested for signs of a chromosomal anomaly. The sample is obtained in one of two ways: by inserting a thin tube (catheter) through the cervix and into the uterus or by inserting a needle through the mother’s abdomen. A local anesthesia is used, and the tube or needle is guided to the placenta by ultrasound. CVS can be performed slightly earlier than amniocentesis, usually between the 10th and 14th week of pregnancy.
What happens after my evaluation is complete?
After we have gathered all the anatomic and diagnostic information from the tests, our full team will meet with you to discuss the results. Lymphatic malformations generally cannot be treated before a child is born. We will, however, take an active approach to managing the condition during your pregnancy. We will monitor both mother and baby very carefully, watching for how the malformation grows and for any potential complications that might develop. We will also watch to see if the malformation shrinks and/or disappears, as they sometimes do.
Sometimes the lymphatic malformation presses against the esophagus and inhibits fetal swallowing. If this occurs, an excess amount of amniotic fluid (polyhydramnios) may occur. In these cases, removal of the excess amniotic fluid — a procedure called an amnioreduction — may be needed to help the mother feel more comfortable. An amnioreduction is similar to an amniocentesis. A small needle is inserted into the amniotic sac under ultrasound guidance, and then some of the fluid is drained away.
The lymphatic malformation may also press against the baby’s airway. If this is suspected, your care team may discuss a special kind of delivery, called the EXIT (Ex-utero Intrapartum Treatment) procedure. An EXIT procedure is a specialized type of cesarean section. The baby is partially delivered while still attached to the placenta. This permits the baby to receive oxygen and nutrients from the mother while the surgeon places a breathing tube into the baby’s airway. Once the tube is in place, the baby can be fully delivered.
If the lymphatic malformation is located elsewhere within the baby, we will monitor that particular area carefully to make sure no damage is occurring. If necessary, we may need to discuss options for early or specialized delivery.
How is a lymphatic malformation treated after birth?
Our goal will be to have your baby’s birth occur as near to your due date as possible, but infants with a large lymphatic malformation must sometimes be delivered early and by cesarean section. Your baby will be born at The Mother Baby Center at Abbott Northwestern and Children’s Minnesota in Minneapolis or at The Mother Baby Center at United and Children’s Minnesota in St. Paul. Children’s Minnesota is one of only a few centers nationwide with a birth center located within the hospital complex. This means that your baby will be born just a few feet down the hall from our newborn intensive care unit (NICU). Also, many of the physicians you have already met will be present during or immediately after your baby’s birth to help care for your baby right away.
Your baby may need specialized medical care after birth, and may therefore be taken to our NICU. For example, if the lymphatic malformation is pressing against your baby’s airway, a mechanical breathing machine (ventilator) may be used to help your baby breathe. If the growth is interfering with your baby’s ability to nurse or take a bottle, your baby may also be placed on special intravenous (IV) lines for the delivery of needed nutrients and medications.
Your baby will undergo further tests after birth to help us make a definitive diagnosis of the extent of the malformation and determine possible treatments. These tests will include advanced imaging techniques, such as ultrasound, MRI and a special type of x-ray known as computed tomography (CT) scanning. CT images are more detailed than standard x-rays.
Once a thorough assessment of your baby’s condition has been made, your comprehensive care team at the Midwest Fetal Care Center will explain the findings to you and what they mean in terms of treatment. The treatment option(s) that will be best for your baby will depend on the size and location of the lymphatic malformation, as well as other factors, including your baby’s overall health, your baby’s ability to tolerate specific medications and procedures, and your overall preferences.
Several treatment approaches are available, including the following:
- Watch-and-wait. In some cases, particularly if the cyst is small or is not threatening an airway, the best treatment approach is to simply keep the malformation under observation. Lymphatic malformations sometimes drain and shrink spontaneously.
- Percutaneous drainage. With this procedure, an incision is made into the lymphatic malformation and the fluid is drained, usually through a small tube (catheter). Percutaneous drainage is usually done in combination with sclerotherapy or surgery.
- This treatment, which is carried out while the baby is under a general anesthesia, involves injecting a special medication into the malformation. The doctor will use ultrasound imaging to help guide the injection of the medication to the right location. The medication ablates (destroys) the cyst, collapsing its walls. The fluid is then drained away through a drainage tube. Sclerotherapy treatments may need to be repeated. Your baby will remain hospitalized until the treatments are completed and there are no signs of swelling of the airways (if the malformation is in the neck or chest area).
- Laser therapy. With this treatment, which is done under general anesthesia, the cysts are destroyed with a strong beam of light. Usually, multiple treatment sessions are needed, spread out over many months. Laser therapy is most often used to treat lymphatic malformations that involve the skin or mucous membranes (the thin layer of skin that lines the nose, mouth and other body cavities and that produces mucus to keep those cavities from drying out).
- Surgical removal. Surgery can be used to remove some lymphatic malformations, particularly those that are small and that do not surround important body parts and organs.
- Medical therapy. In some cases, medications are used to treat lymphatic malformations. One such medication is sirolimus, a drug used by organ transplant patients to keep their immune system from rejecting their new organ. One of the effects that sirolimus has on the body is to suppress the uncontrolled growth of blood vessels within the lymphatic system. By suppressing that growth, the medication shrinks existing lymphatic malformations and prevents the formation of new ones.
What is my baby’s prognosis?
In the absence of genetic anomalies, the prognosis for babies born with lymphatic malformations is excellent. They have normal, active, happy lives. Outcomes are more variable for babies born with genetic anomalies. Their prognosis depends on the extent of the anomaly.
Will my baby require long-term follow-up?
Because of the potential health issues associated with lymphatic malformations and because treatments must often be repeated, your baby is likely to require long-term follow-up care. At Children’s Minnesota, we will work with you to develop a detailed care plan for your baby. Your baby’s plan will be implemented by a comprehensive team of specialists under the overall coordination of a pediatrician.
Contact us
Need a referral or more information? You or your provider can reach the Midwest Fetal Care Center at 855-693-3815.